Case 34
Shortness of breath in an elderly woman with COPD and obesity
Preview:
Please login, activate your subscription,
or explore access solutions.
Brief History of Present Illness
The patient was an obese, elderly Caucasian woman with history of hypertension, diabetes, atrial fibrillation (on Coumadin), COPD, asthmas, and May Thurner syndrome (status post recent stent placement in the left iliac vein), who presented to the emergency room after waking up in the middle of the night with shortness of breath.
This was not relieved by multiple nebulizer treatments at home.
She could not lie flat because she felt “breathless.”
She also complained of left-sided chest plain.
There was no fever or upper respiratory symptoms.
Hospital course
On admission, Troponin I, POC was 3.18 ng/mL and BNP was 754.9 pg/mL.
She was diagnosed with a non-ST elevation myocardial infarction and treated with IV heparin and beta blockers.
On hospital day 2, Troponin I levels were 3.85 and 3.02 ng/mL.
First cardiac catheterization
On hospital day 3, the patient underwent a cardiac catheterization.
Left heart catheterization procedure note and diagram
Page 1
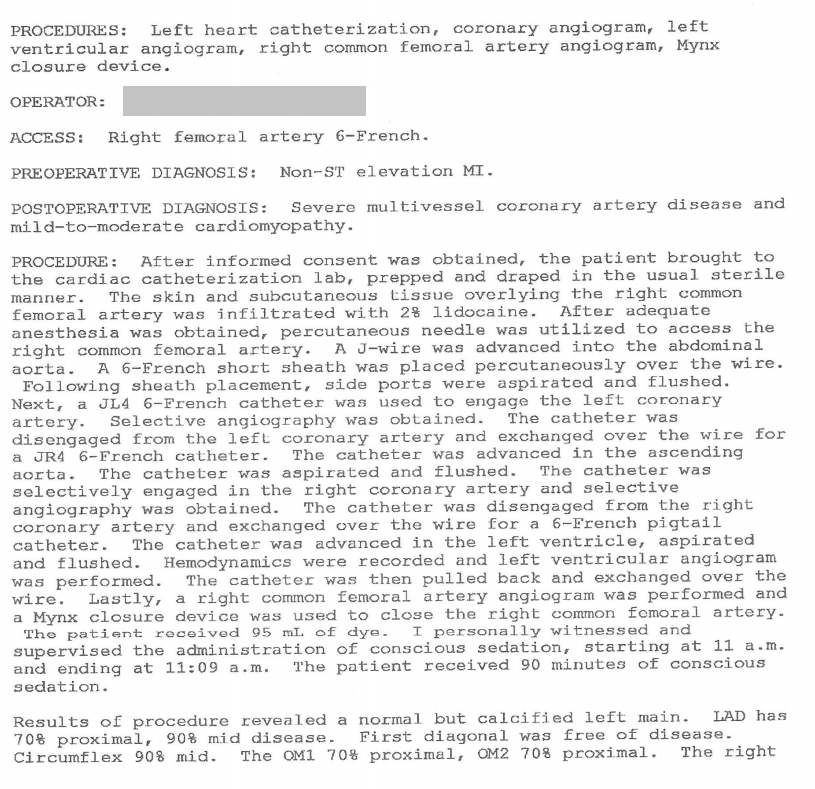
Page 2
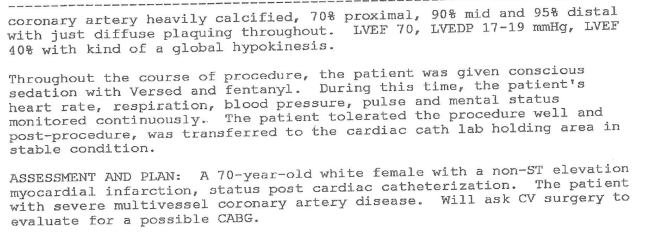
Diagram
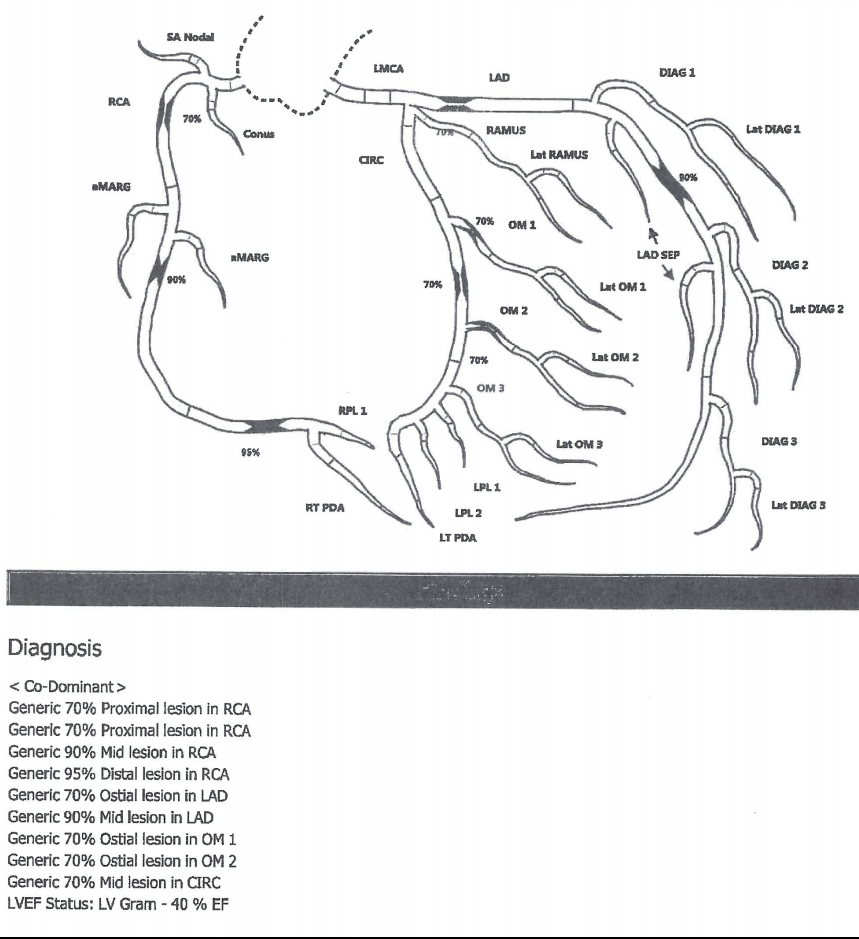
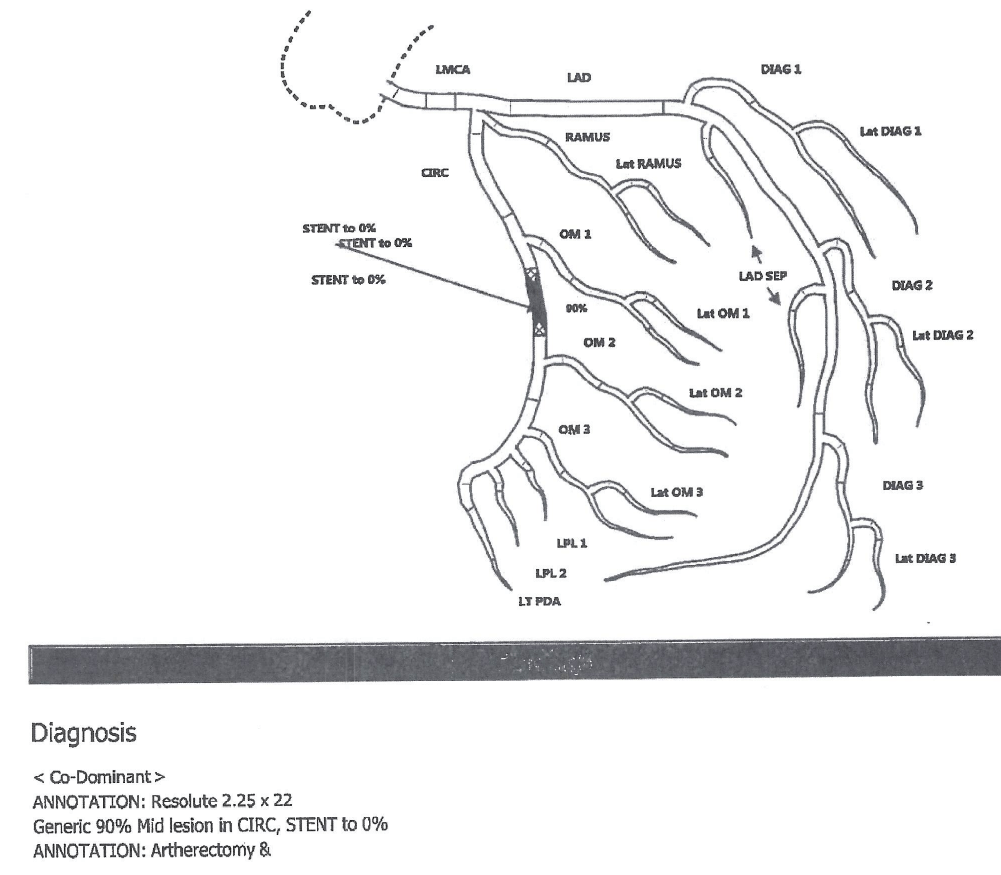
Second cardiac catheterization
She was deemed not a candidate for bypass surgery (due to her lung condition) and instead underwent coronary stent placement (hospital day 5).
Second left heart catheterization (with stent placement) procedure note and diagram
Page 1
Page 2
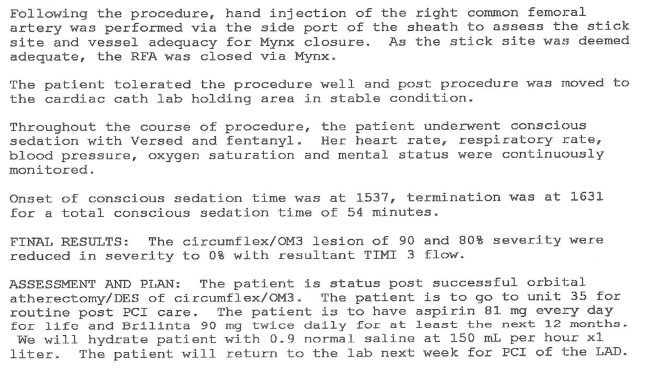
Diagram
Immediate post-catheterization
The patient was stable in the immediate post-operative period
Later in the day
Later that day, the nurse was unable to find a pulse in the right foot.
The patient was agitated with some mental status changes.
She notified the physician of both issues.
Physician assessment
The physician found the patient to be tachypneic and short of breath, with no pulse on the right foot by doppler and also complaining of groin pain.
The patient was saturating 82% on room air.
He noted a possible right groin hematoma.
An ultrasound was to be ordered to rule out hematoma, per the physician note.
The patient was placed on a nonrebreather mask with improved oxygen saturation to 99% by arterial blood gas.
The patient’s tachypnea was attributed to anxiety and the patient was prescribed Ativan.
Overnight
Throughout the evening and overnight the patient remained somewhat confused.
The following morning
In the morning (hospital day 6) the patient was found hypotensive with a rigid abdomen.
She was intubated emergently.
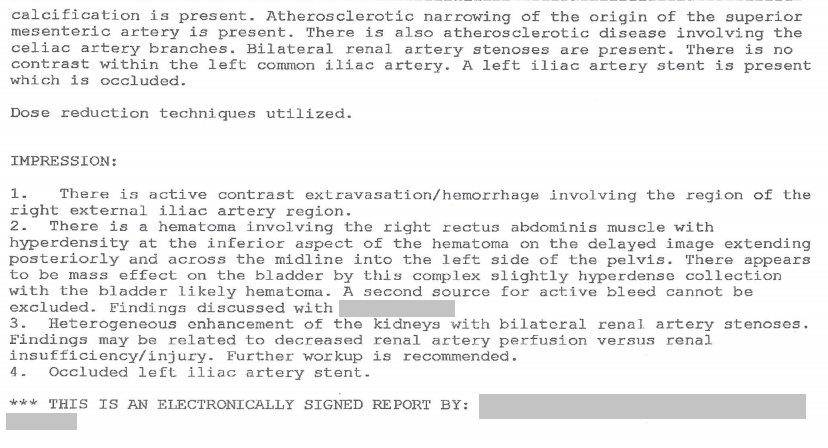
The patient had a CT of the abdomen and pelvis with contrast.
There is no record of an ultrasound being performed by this time.
Results of CT Abdomen and Pelvis
Page 1
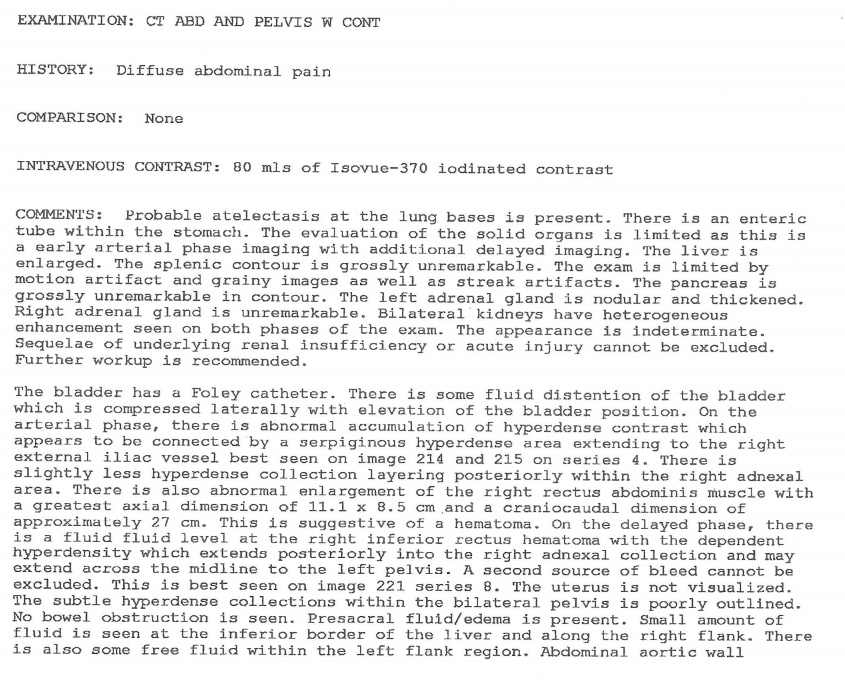
Page 2
Placement of stent/patch
The patient underwent abdominal aortography with placement of a patch.
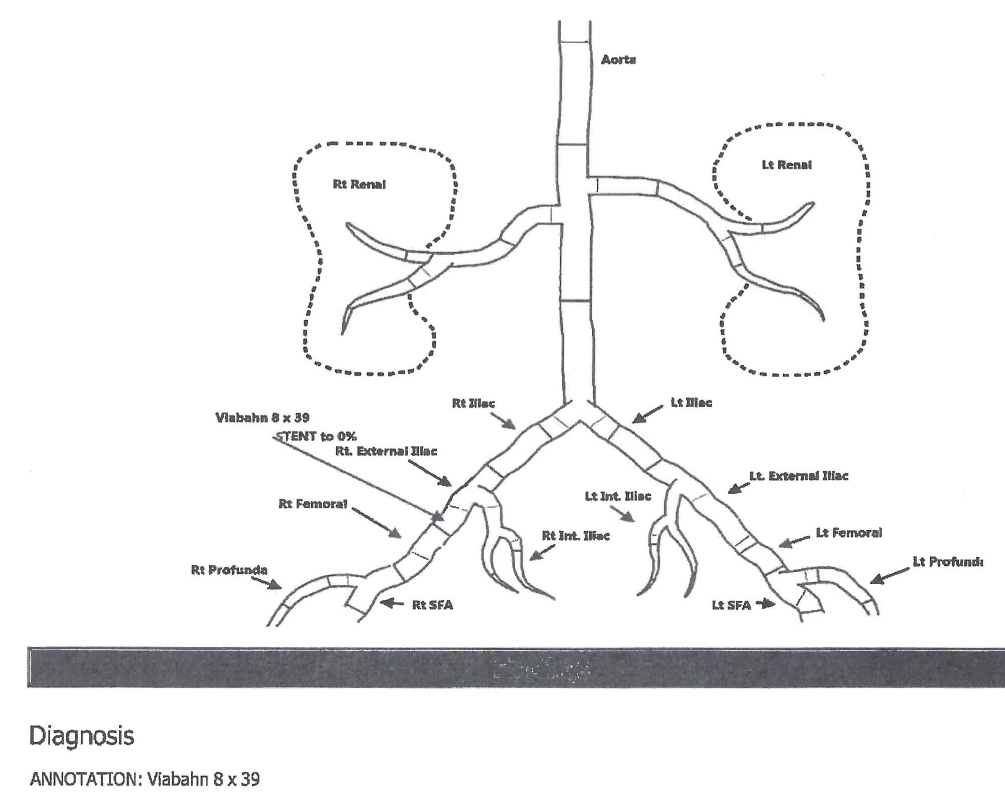
Abdominal aortography procedure note and diagram
Page 1
Page 2
Diagram
Hospital course (continued)
The patient could not be stabilized, required 10-15 units of blood over the next several hours and died.
Discussion Questions
1. Summarize the history.
2. What is the differential diagnosis of sudden onset of shortness of breath in the patient with obesity and COPD?
3. How many cardiac catheterizations did the patient have?
4. How does a cardiac cath work?
5. What is a coronary stent?
6. What medical conditions are associated with obesity?
7. What steps would you take to safely lift, turn, or transport a patient of this size?
8. What surgical risks increase for obese patients?
9. How much more difficult is it to insert a catheter into the groin of an obese patient than a thin patient?
10. What key medical errors were made in this case? What would you have done differently? (Revisit this question after viewing the entire case. Did your answer change? If so, why?)
11. The nurse diligently reported a key postoperative clinical finding to the physician. What was that key finding?
12. After learning a key postoperative clinical finding, the physician made an assessment that did not address a life-threatening issue. Why do you think this happened? What internal, relationship, or training factors might explain this outcome? How might this be addressed with this physician?
13. When does the nurse’s role extend beyond reporting of critical information? What is the nurse’s role when the physician makes a determination that puts the patient at risk? What is a team’s role when a key member makes an error, does not address issues competently, or puts a patient’s life at risk?
