Case Histories
Scroll down to start
↓
Then select case above.
Look for the magnifying glass:
to magnify text.
The patient was an active, elderly Caucasian woman on hypertensive medication, recently hospitalized for pneumonia….
![]()
Case 1
(Click to view all parts)
Recent pneumonia
Preview:
Case 1 – History 1
Brief History
The patient was an active, elderly Caucasian woman on hypertensive medication, recently hospitalized for pneumonia.
She lost 10 pounds in the hospital.
She completed her antibiotic course at home and was recovering, with a residual cough.
She was found dead facedown on the floor after an unwitnessed cardiopulmonary arrest approximately two weeks after discharge.
The history is obtained from the family.
Discussion Questions
2. Do you think the patient fully recovered from her pneumonia?
3. How would your answer change if the patient had died one day after discharge from the hospital?
4. What are appropriate discharge instructions after hospitalization from a pneumonia?
Back to history
Case 2
(Click to view all parts)
Diabetes, stroke, feeding tube
Preview:
Case 2 – History 1
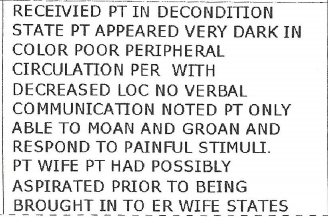
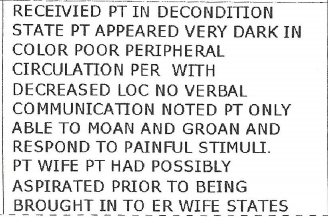
Brief History of Present Illness
The patient was a middle-aged African American man with insulin-requiring diabetes (with multiple admissions for diabetic ketoacidosis), stroke (with immobility and difficulty swallowing, requiring gastrostomy and jejunostomy tube placement), hypertension and dementia who was noted to have a high blood glucose and lethargy as well as shortness of breath and cough for a couple days.
Case 2 – History 2
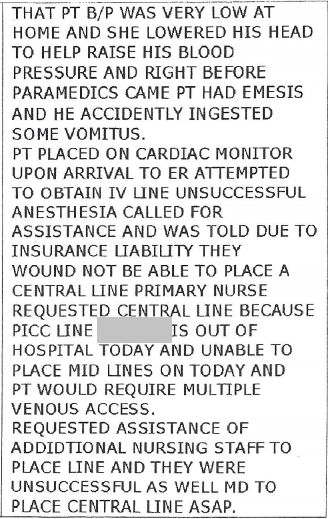
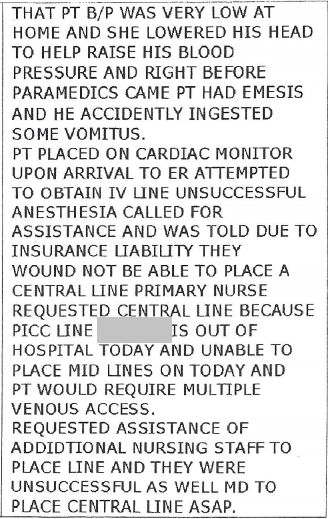
Home Events
The wife took his blood pressure, which was “very low,” lowered his head to help raise his blood pressure and called paramedics.
Right before they came, the patient vomited.
The wife was concerned he accidentally “ingested” some vomitus.
Case 2 – History 3
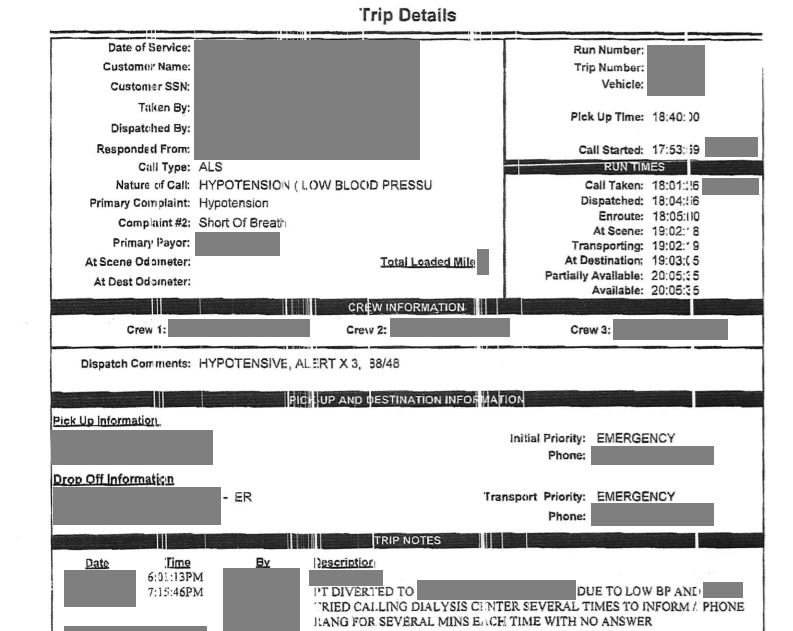
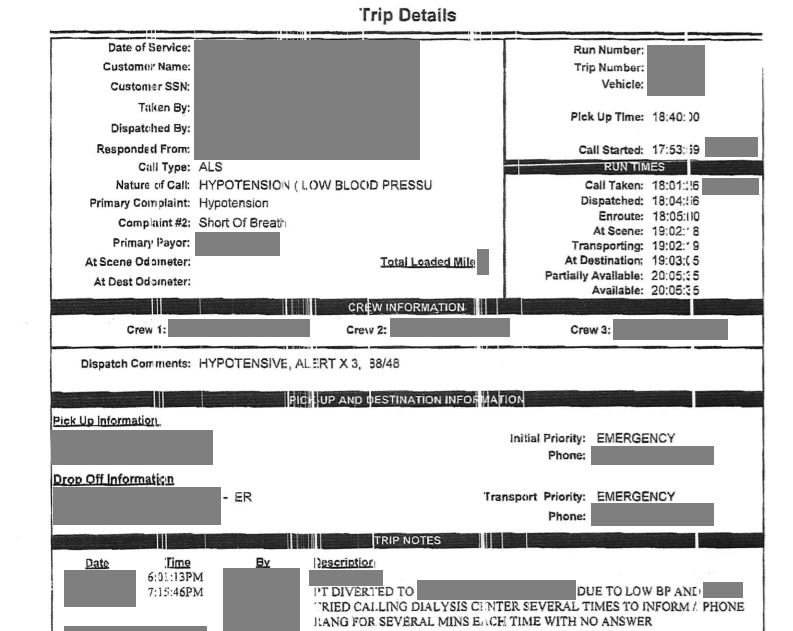
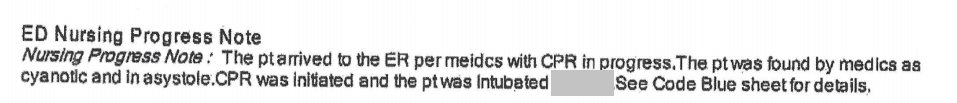
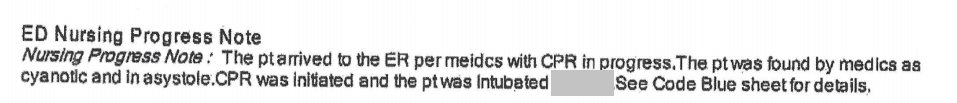
Paramedic Notes
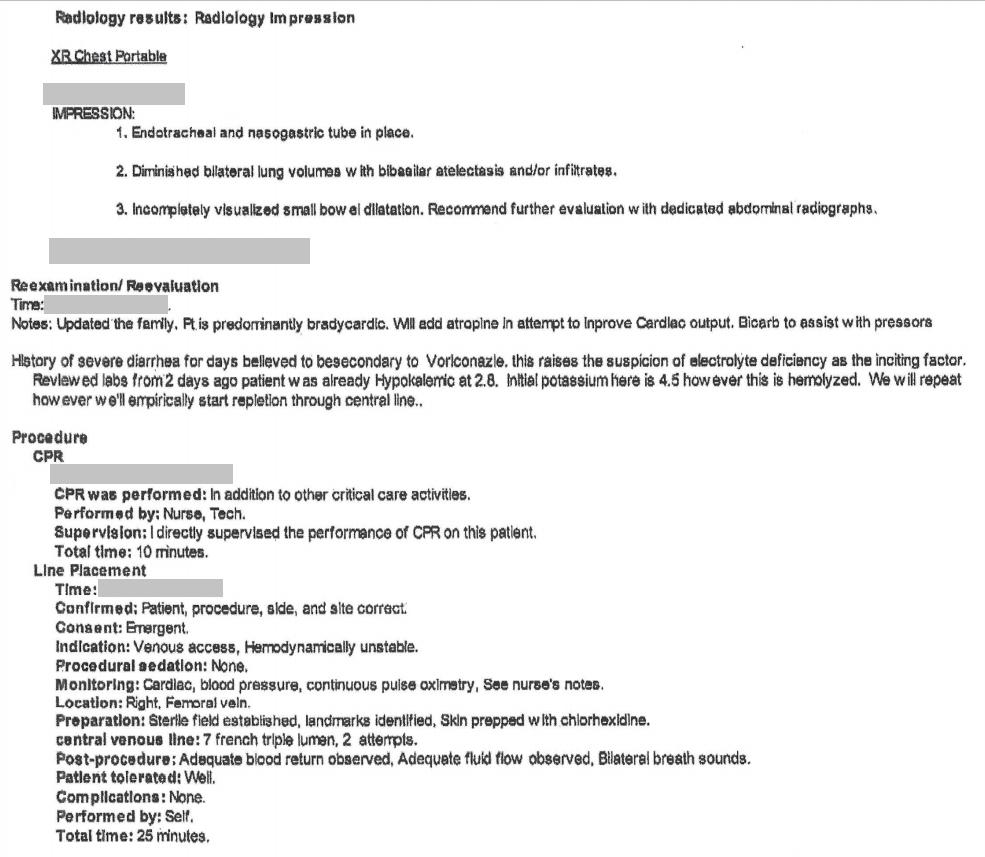
![]()
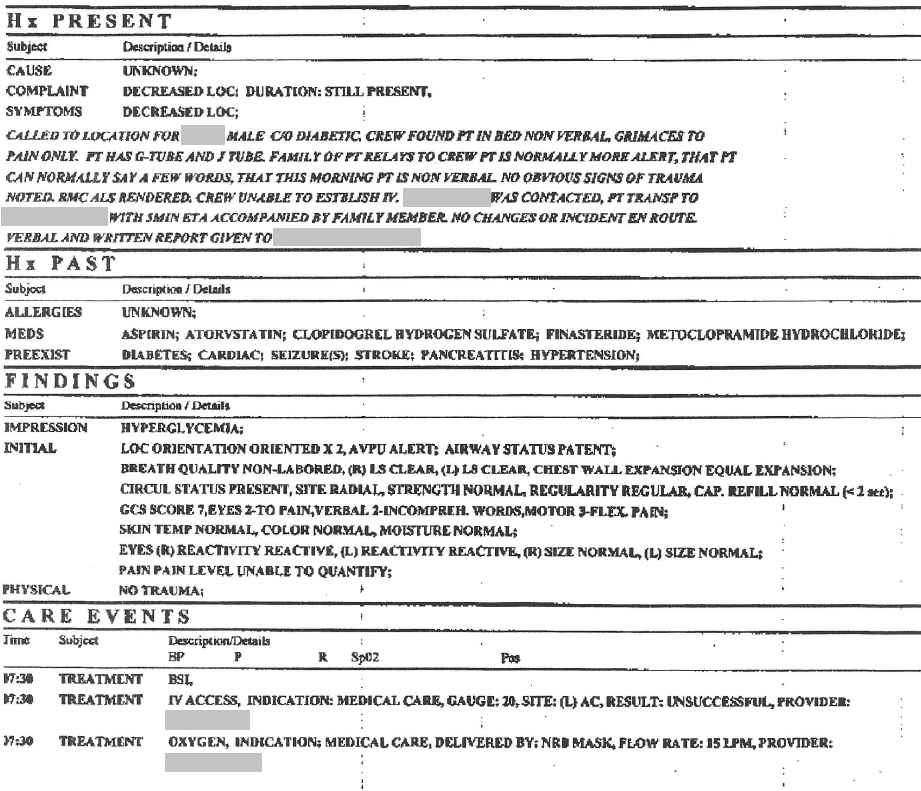
Page 2
![]()
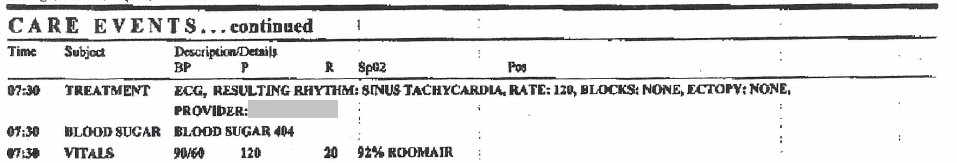
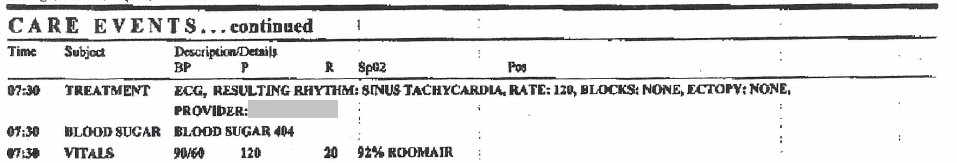
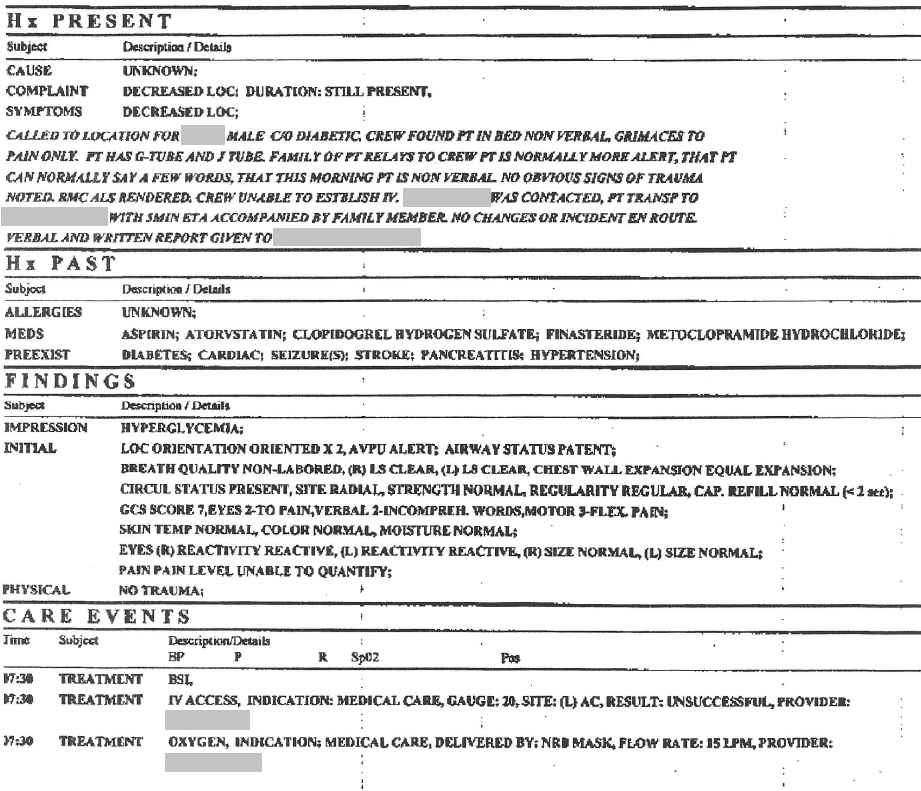
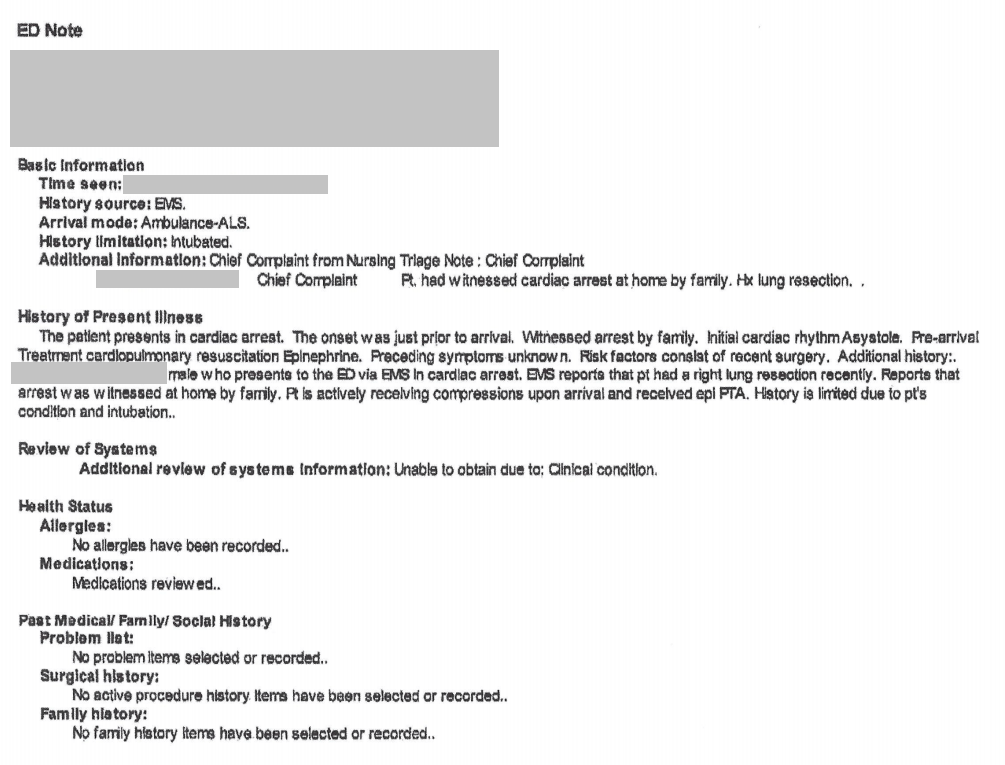
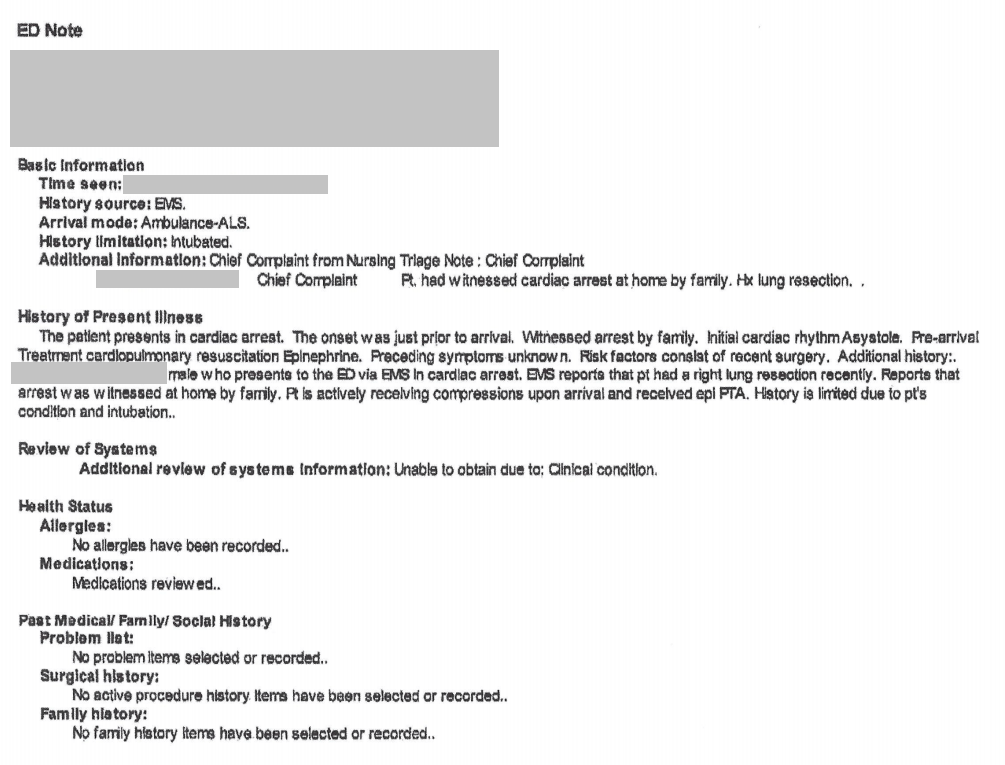
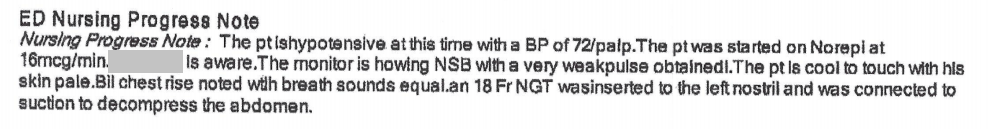
Case 2 – History 4
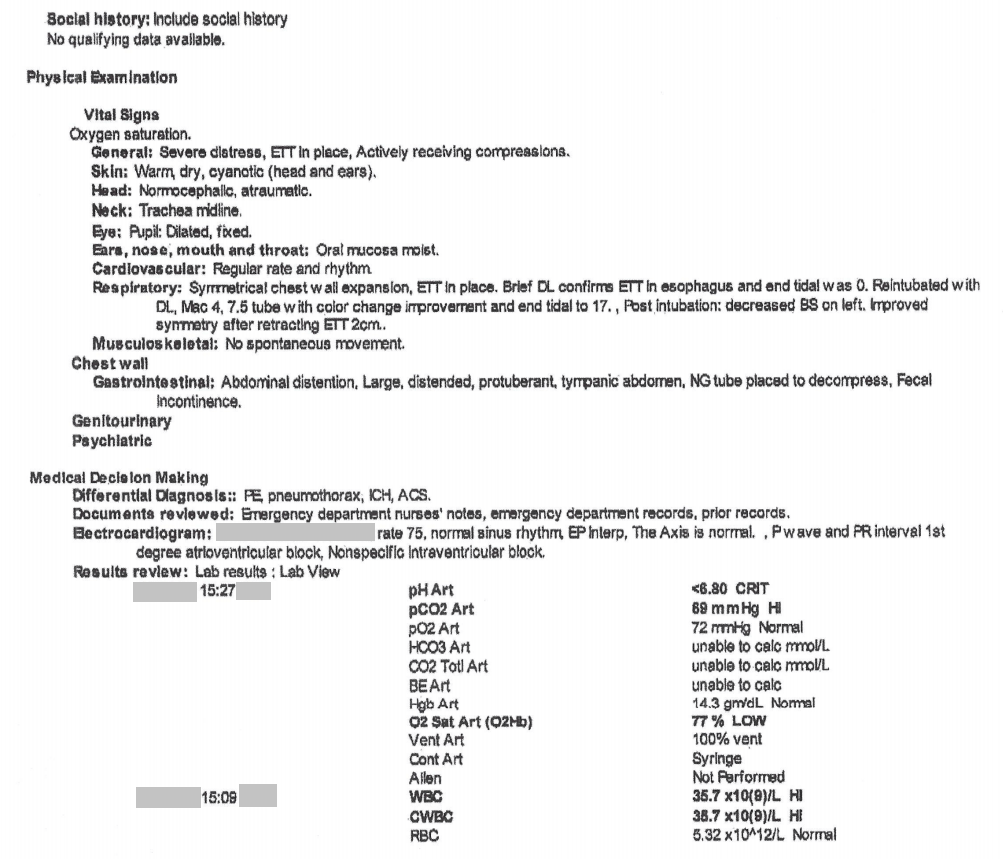
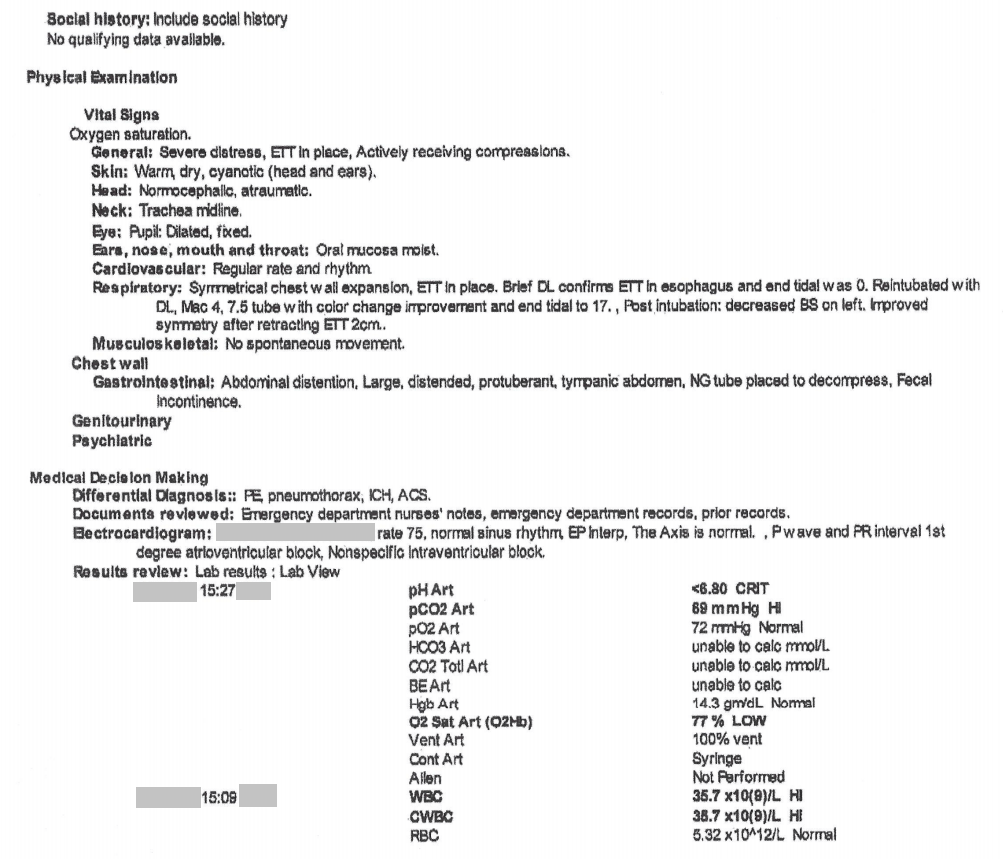
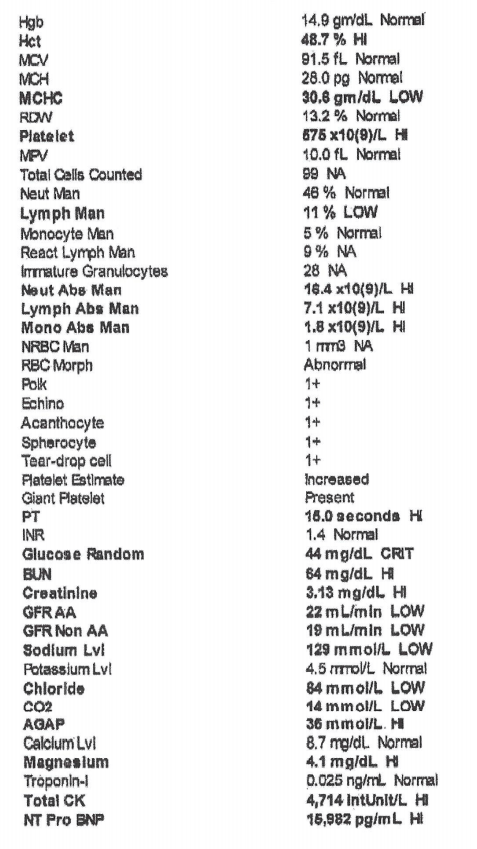
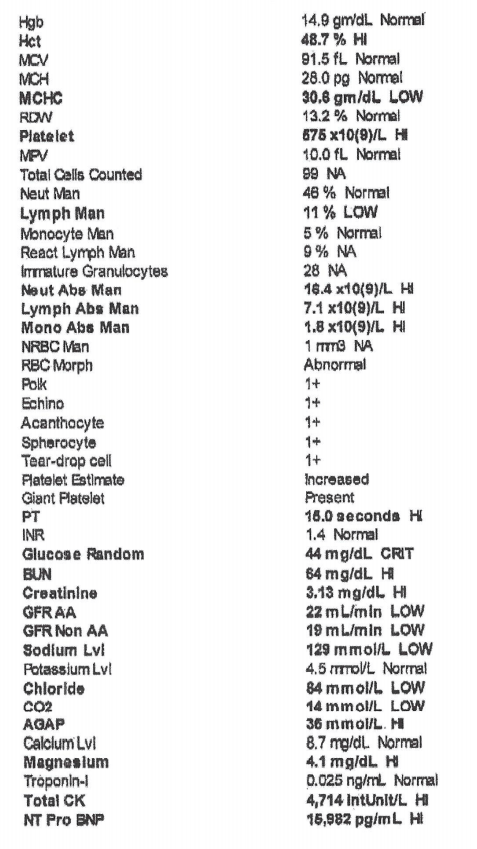
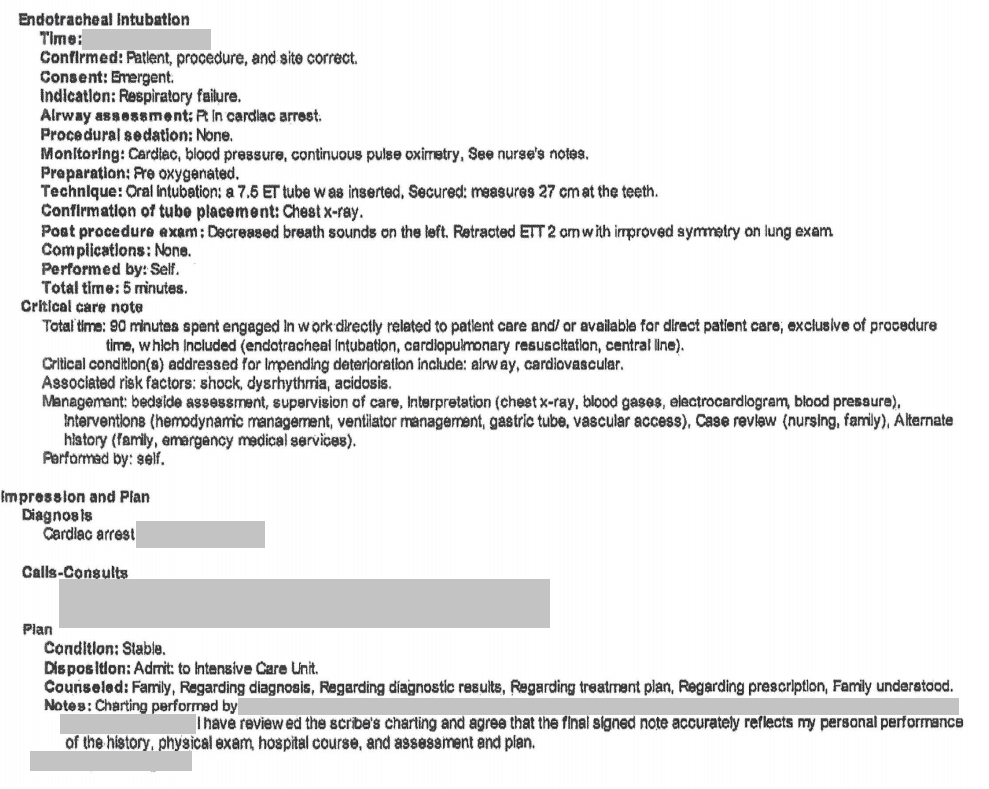
Emergency Room Note
![]()
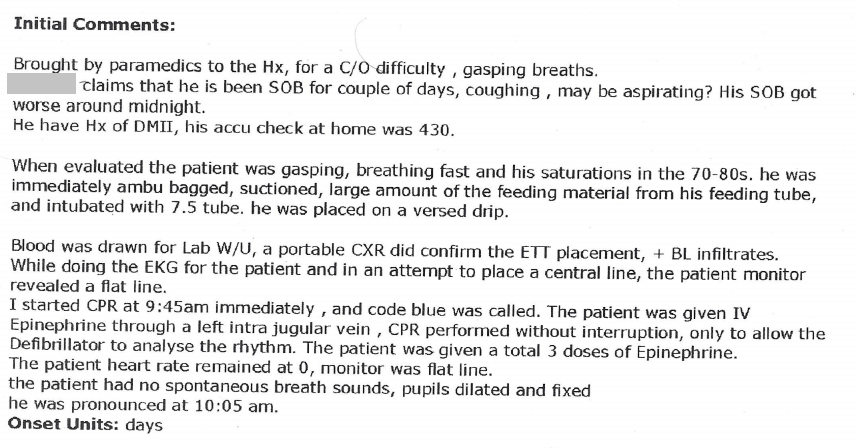
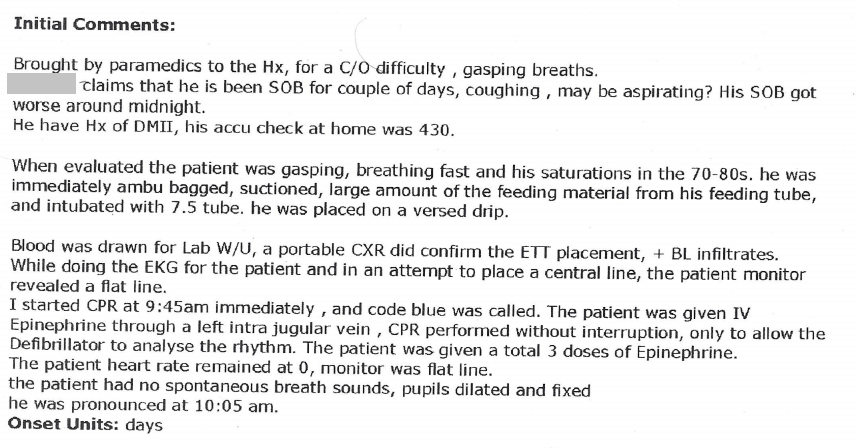
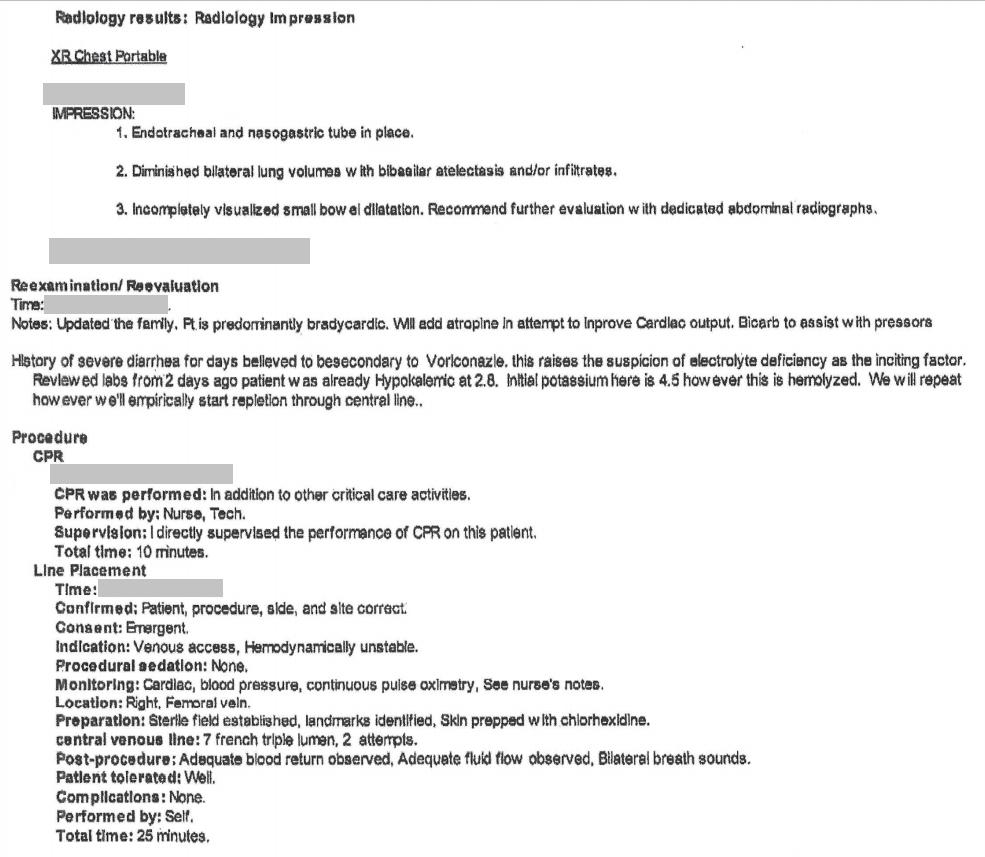
Case 2 – History 5
Additional Emergency Room Note
Intubation was difficult requiring three attempts with varying size endotracheal tubes.
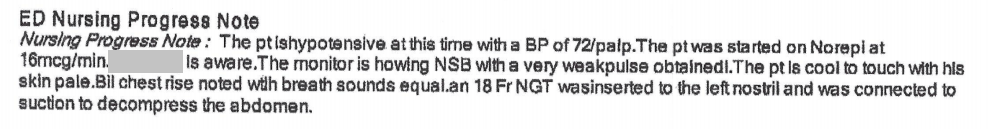
Case 2 – History 6
Additional Emergency Room Note
![]()
Page 2
![]()
Case 2 – History 7
Additional Emergency Room Note
The patient died in the emergency room.
Discussion Questions
2. What was the patient’s status upon arrival of paramedics? During transport? In the emergency room? Are there any discrepancies? If so, how do you account for them? (See medical records.)
3. What choices affected the patient’s care starting from home through to the emergency room?
4. Are there any choices that were intended to help but which may have led to worsening of his condition?
5. What is your opinion on “assigning fault” in a death? How would you talk with someone who intended to help a patient, but ended up harming them? What if this were a family member? Does any of this apply to this case? How?
6. What ethical issues are raised in the medical record titled “View additional emergency room note”?
7. The history states there were three attempts at intubation. What factors can make intubation difficult? List ones that are related to the patient. List ones that are related to the provider.
8. Create your own definition of what it means to be a “competent” health care provider. Can you imagine an adverse outcome with “competent care”?
9. Come back to questions 1 – 8 after studying the videos and decide if you wish to revise any of your answers.
Back to history
Case 3
(Click to view all parts)
Recent chest pain
Preview:
Case 3 – History 1
Brief History
The patient was a middle-aged Caucasian man with history of heavy smoking and recent left rib pain (medicated with ibuprofen) who was found dead after an unwitnessed collapse.
Last contact with the family was one day prior.
Discussion Questions
2. What is your differential diagnosis for the patient’s symptoms? For a cause of death?
Back to history
Case 4
(Click to view all parts)
Transdiaphragmatic tumor
Preview:
Case 4 – History 1
Brief Past Medical History
The patient was an elderly man in prior excellent health with history of possible asbestos exposure in the early 1970’s at a utility company.
He was admitted approximately one month prior with diagnosis of pneumonia.
The patient’s father died at age 68 of myocardial infarction.
There is no history of cancer in the family.
Case 4 – History 2
Hospital course
He was found to have a mass in the left chest that protruded through the rib cage under the skin.
It was determined radiographically to be of origin from the abdominal peritoneum, extending through the diaphragm and into the anterior chest wall under the skin.
A secondary mass was identified under the sternum, possibly adherent to the pericardial fat.
Initial biopsy was inconclusive.
A follow-up biopsy showed sarcomatoid malignant mesothelioma.
This history is obtained from the family.
Discussion Questions
1. Summarize the patient history.
2. Was the patient’s cancer detected early or late in its course?
3. When a patient presents with advanced cancer, what does this tell you about their self-care (if independent) or clinical care (if dependent)?
4. What factors need to be in place for a patient to be able to detect and seek care for a condition like cancer? How could you, as a provider, assist your patients in this process?
5. What is the connection between smoking and asbestos when it comes to cancer?
Back to history
Case 5
(Click to view all parts)
Dementia
Preview:
Case 5 – History 1
Brief History
The patient was an elderly Caucasian man with longstanding undiagnosed dementia.
Discussion Questions
2. Why would a family want to make a specific diagnosis postmortem?
3. How can you distinguish the difference between inherited and sporadic forms of dementia?
Back to history
Case 6
(Click to view all parts)
Spinal surgery
Preview:
Case 6 – History 1
Brief History
The patient was an elderly Caucasian woman with rheumatoid arthritis, medication-controlled hypertension, and managed unspecified kidney disease (evaluated yearly), who underwent elective spinal fusion surgery for lumbosacral spinal stenosis after cardiology clearance (by echocardiogram and angiogram).
Case 6 – History 2
Hospital course
The surgery was complicated by altered mental status in the immediate postoperative period with concern for medication effect.
However, the symptoms did not change after medications were discontinued.
The postoperative course was further complicated by multiple falls, a back infection requiring multiple surgeries, and eventually concern for a central nervous system infection.
Case 6 – History 3
Hospital course (continued)
A lumbar puncture could not be performed due to the recent surgery.
A cervical puncture was instead performed with adequate retrieval of cerebrospinal fluid sample, but inconclusive results.
Subsequently, a temporary anterior forehead shunt was placed to retrieve spinal fluid with unknown results.
The shunt was removed.
Case 6 – History 4
Hospital course (continued)
The patient’s conditioned remained stable, but poor for the next month.
She was made do not resuscitate with comfort measures and then died approximately two months after her initial spinal surgery.
The history is obtained from the family.
Discussion Questions
1. Summarize the history.
2. The history suggests one explanation for the post-operative confusion. What other explanation might there be? (What is the differential diagnosis of post-operative confusion?) What clinical data would you want to see to confirm you thought?
3. The history states the confusion did not resolve on discontinuing of medication. If you were the provider, how would you discuss this with the family and what explanations might you then offer for the patient’s confusion.
4. How is spinal fusion surgery performed?
5. What informed consent risks would you cover for a patient with this type of surgery?
6. Based on the history, why do you think the patient had post-operative complications? Can you draw any conclusions about the cause of the infection?
Back to history
Case 7
(Click to view all parts)
Inferior vena cava filter
Preview:
Case 7 – History 1
Brief Past Medical History
The patient was a middle-aged Caucasian man with hypertension and obesity who had a prior head injury from a fall down stairs eight years prior with acute intracranial bleeding requiring craniotomy; and long-term complication of seizures treated medically.
He had a temporary inferior vena cava filter placed prophylactically.
The filter became embedded into the inferior vena cava wall and could not be surgically removed.
He presented for medical attention two months before death with shortness of breath.
Cardiovascular and infectious (viral) work-up were negative.
Case 7 – History 2
Day of Death
On the day of death, he was noted to be sweating and with a right-sided droop.
The patient then collapsed, had a possible seizure and died.
Discussion Questions
1. What are short- and long-term sequelae of traumatic brain injury (such as the patient had)?
2. What is the purpose of an inferior vena cava filter?
3. Under what circumstances is this type of filter placed?
4. What are complications of placing an inferior vena cava filter? Which one did this patient have?
5. When is inferior vena cava filter placement temporary? When is it permanent?
Back to history
Case 8
(Click to view all parts)
TIPS procedure
Preview:
Case 8 – History 1
Brief Past Medical History
The patient was a middle-aged man with prior alcohol use disorder with cirrhosis; and chronic renal disease of unknown etiology on peritoneal dialysis.
The patient was evaluated for kidney vs. kidney-liver transplant.
Transplant was deferred to due elevated transhepatic pressure.
The patient was first scheduled for a transjugular intrahepatic portosystemic shunt (TIPS) procedure.
Case 8 – History 2
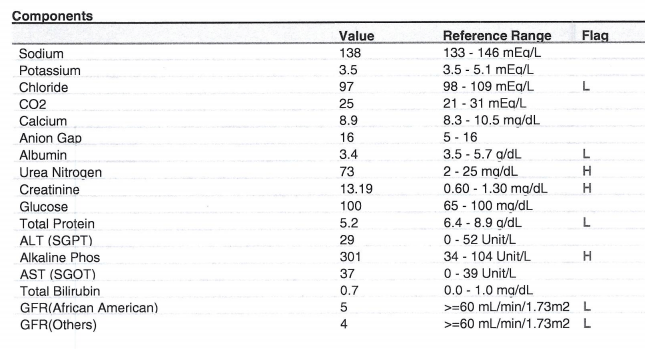
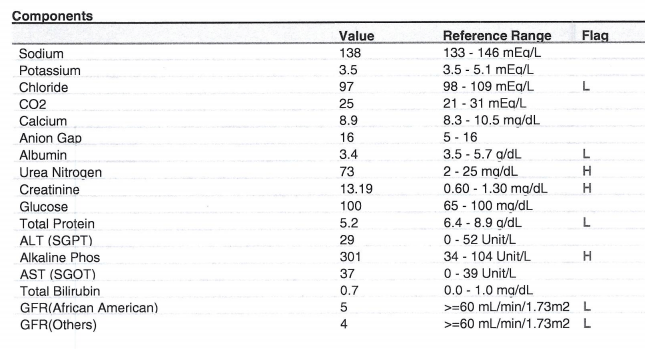
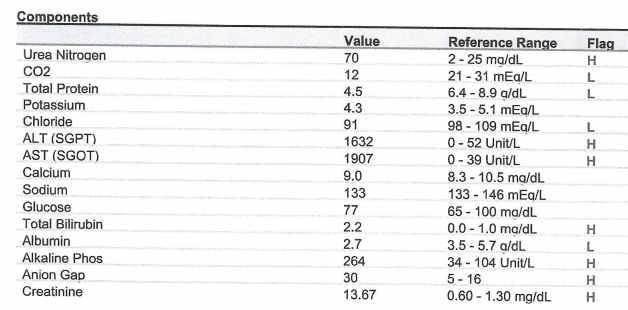
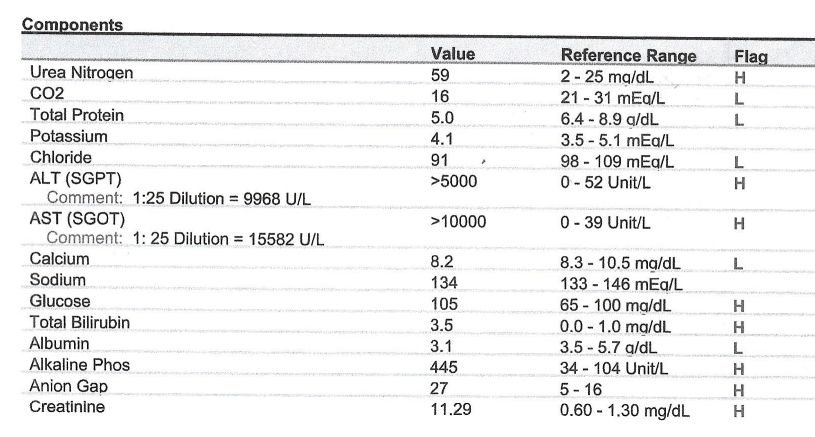
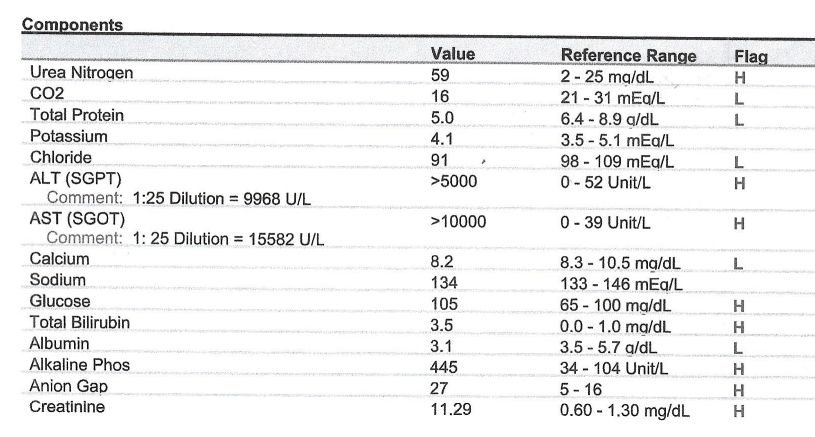
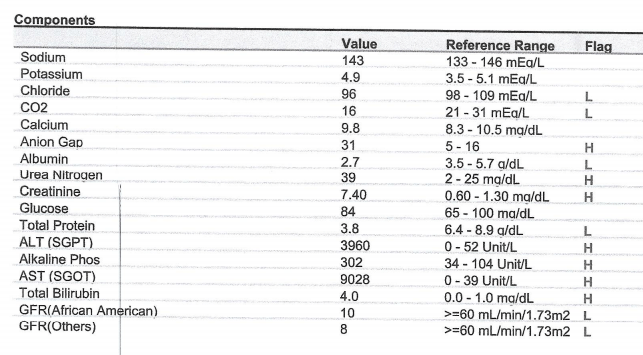
Pre-operative labs
![]()
Case 8 – History 3
Hospital course
The patient underwent the TIPS procedure.
Case 8 – History 4
TIPS Fluoroscopy
Case 8 – History 5
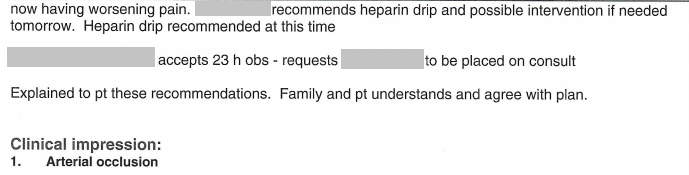
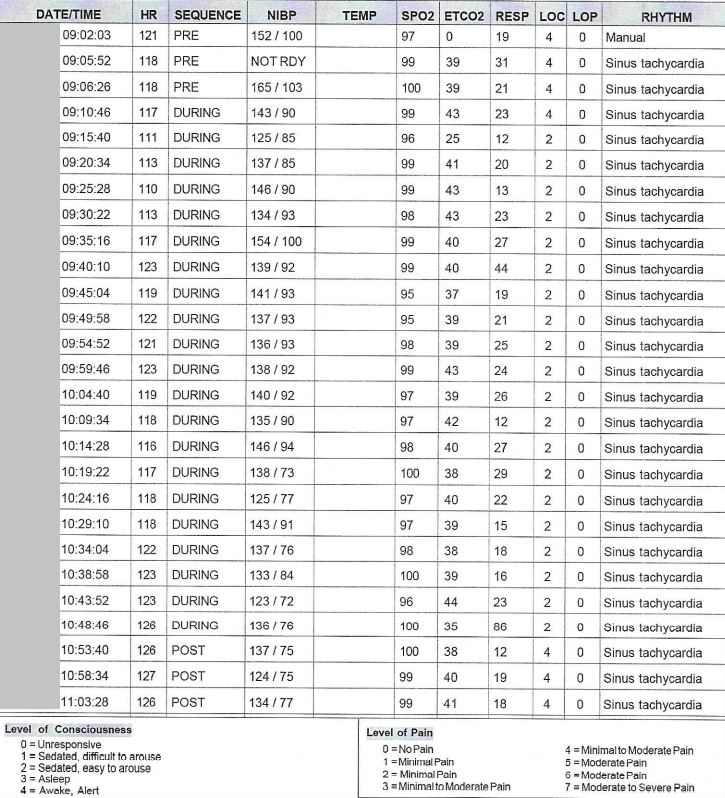
Intraoperative events
The procedure was complicated intraoperatively by a duration of hypotension during repositioning to a transplenic approach.
Case 8 – History 6
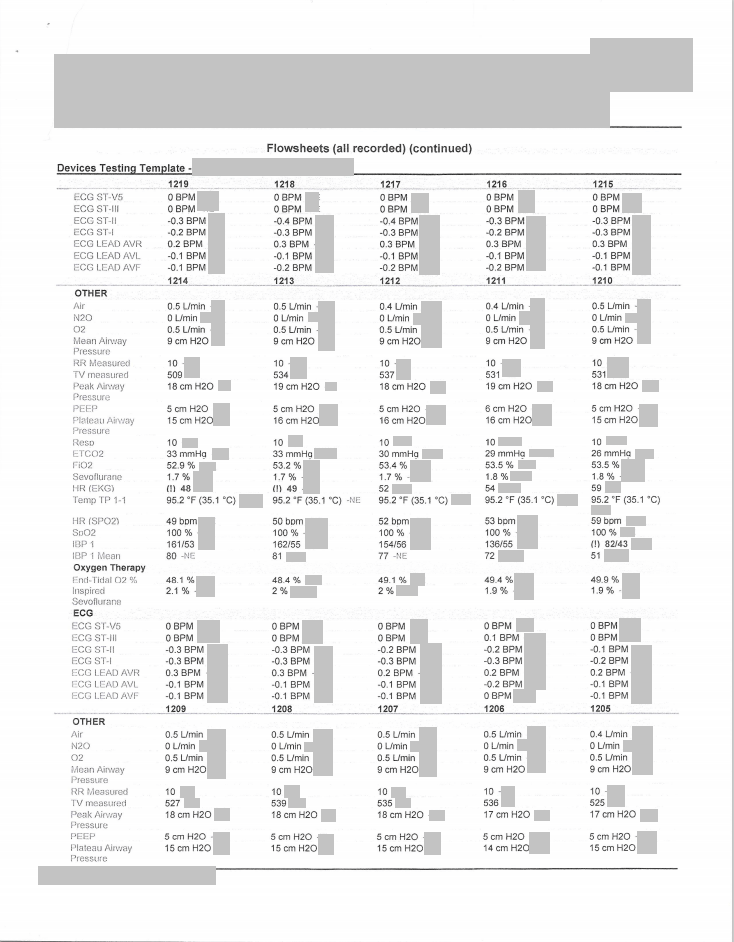
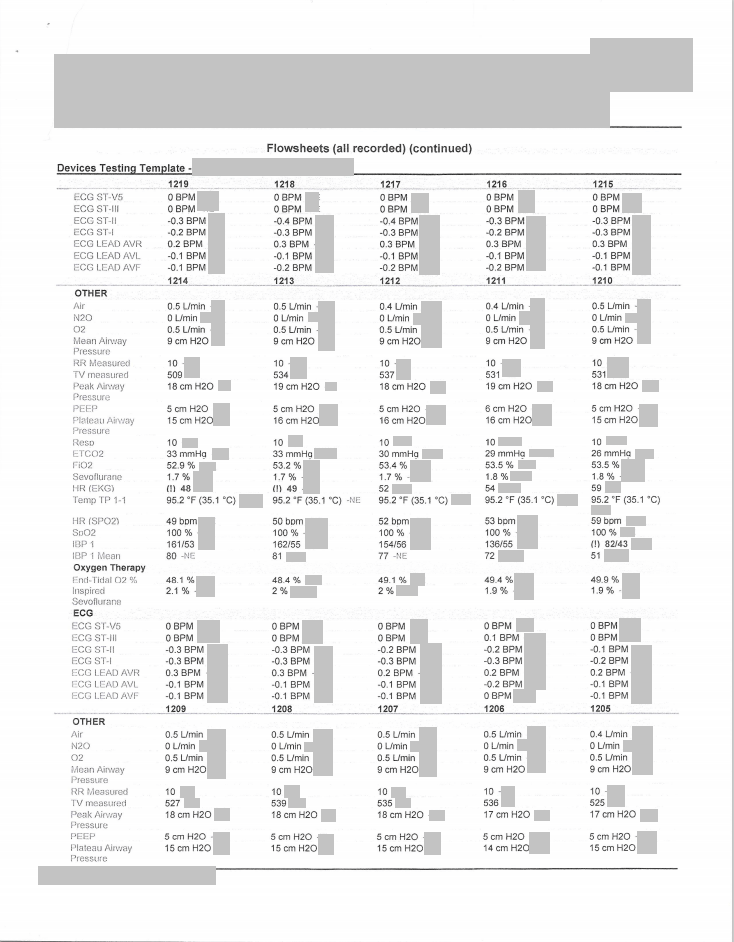
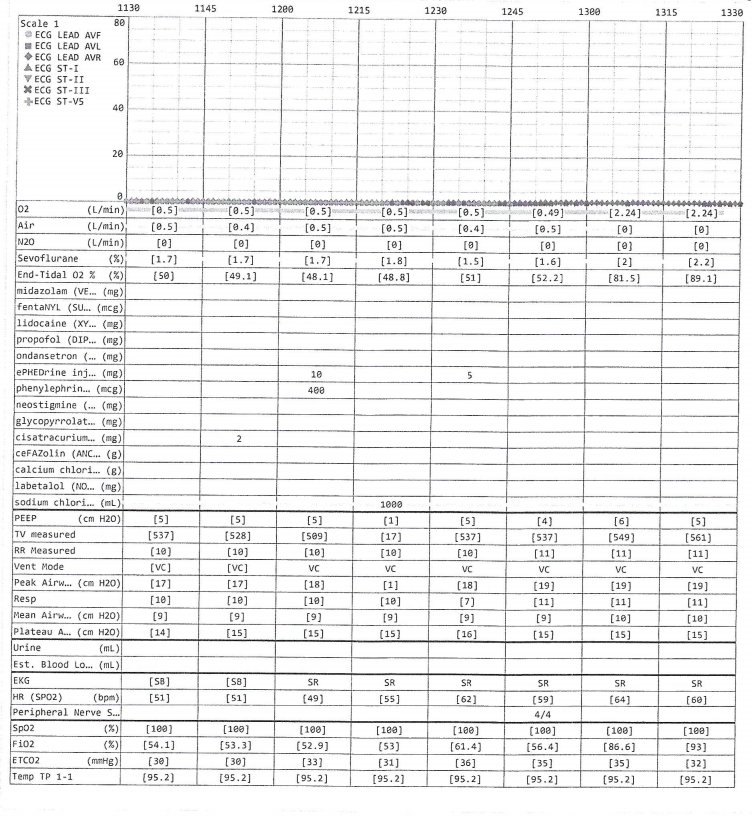
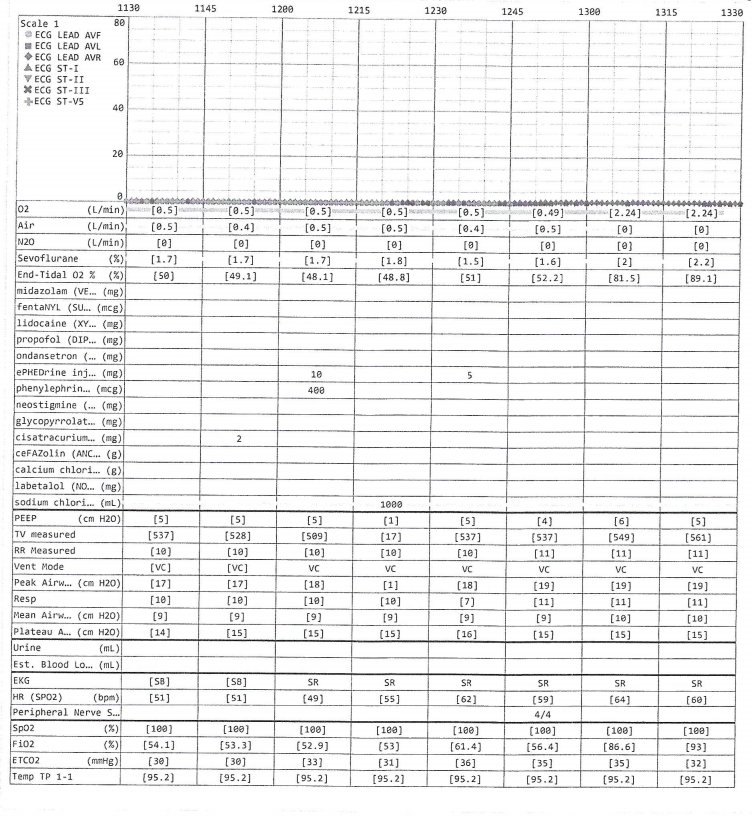
Selected Anesthesia Data
Page 1 of 2
![]()
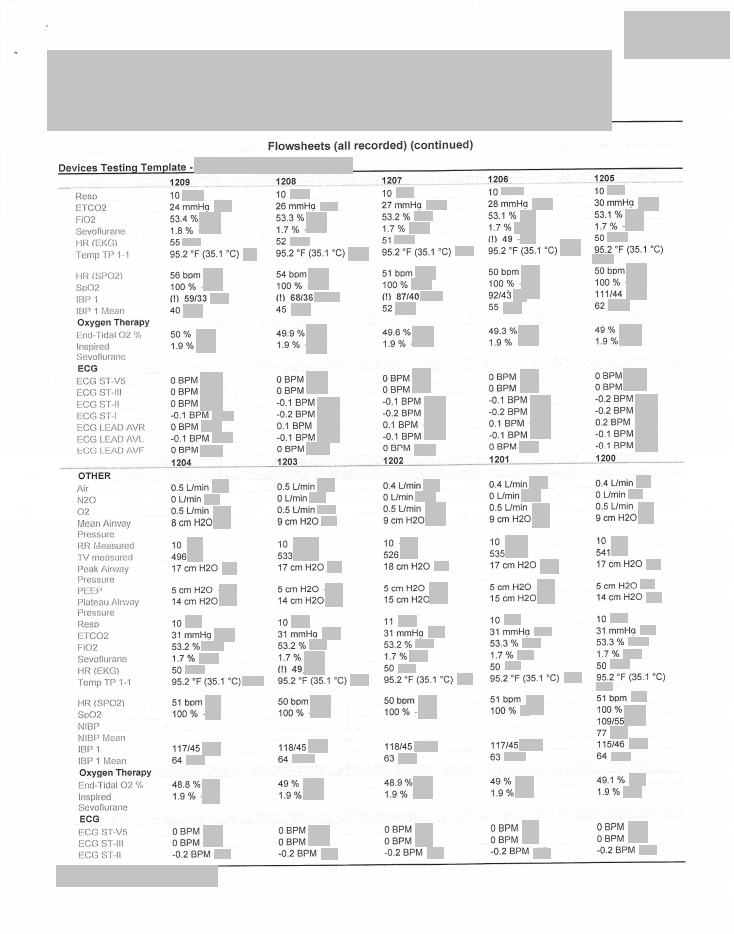
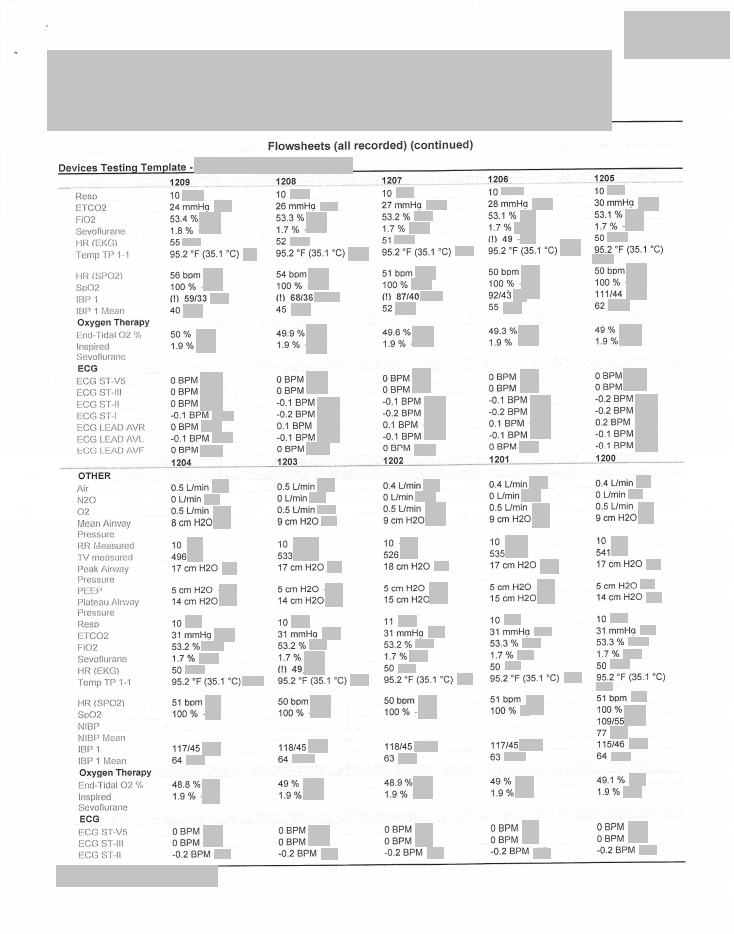
Page 2 of 2
![]()
Case 8 – History 7
Portion of Anesthesia Graph
Page 1 of 2
![]()
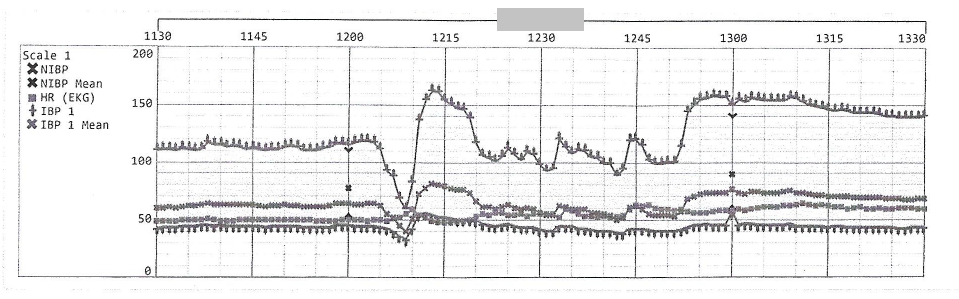
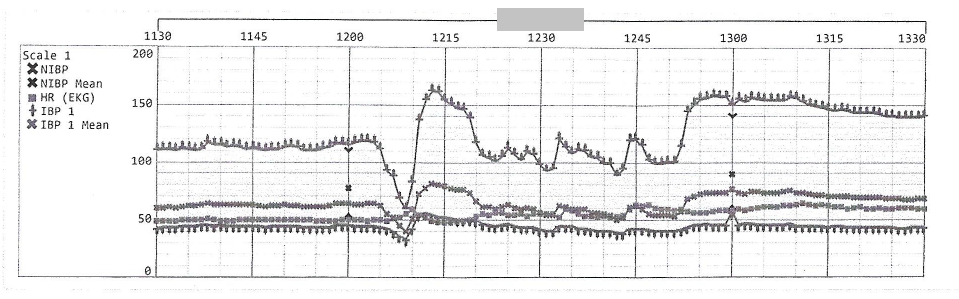
Page 2 of 2
![]()
9
Case 8 – History 9
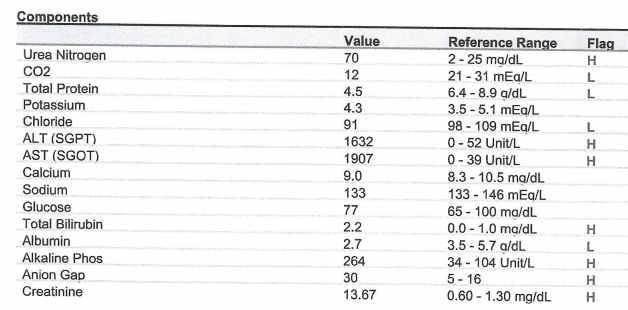
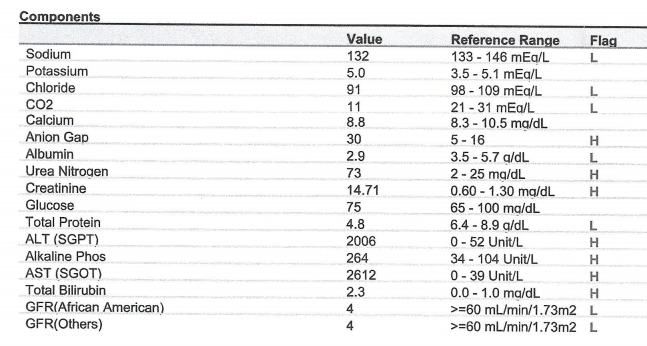
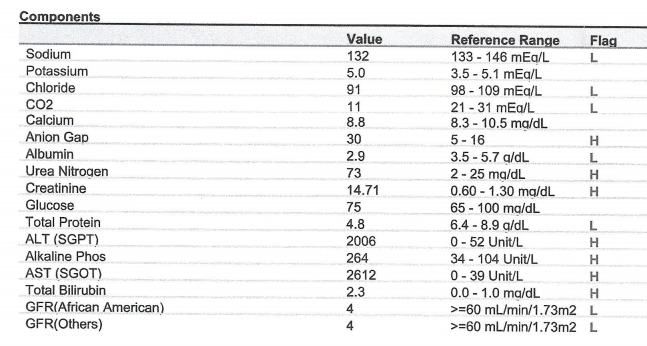
Postoperative course
Careful Review of the medical records showed no documentation that any members of the post-operative care team were aware of the intraoperative hypotension.
Case 8 – History 10
Postoperative Labs – POD 1
POD 1 0225
![]()
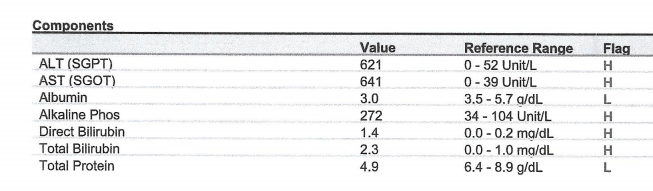
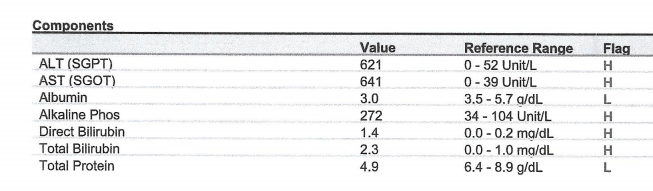
POD 1 0708
![]()
POD 1 0815
![]()
POD 1 2233
![]()
Case 8 – History 11
Postoperative Abdominopelvic CT – POD 1
AXIAL view
(switch to coronal view)
(Start at 02:18 for rapid view.)
CORONAL view
(switch to axial view)
(Start at 03:52 for rapid view.)
Case 8 – History 12
Postoperative Labs – POD 2
![]()
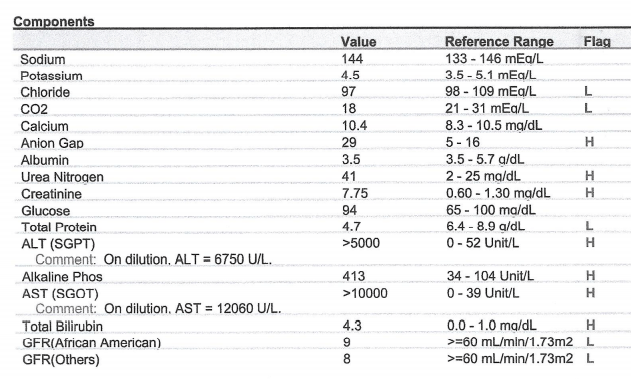
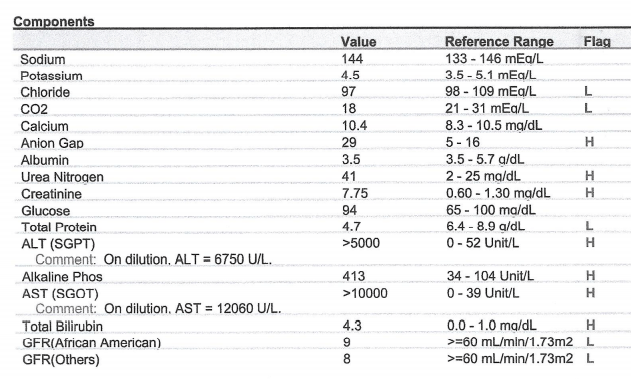
POD 2 1201
![]()
Case 8 – History 12
Postoperative course, continued
The post-operative course was complicated by progressive elevation in liver function test, hepatic failure and then multi-organ failure in the immediate postoperative period.
The patient underwent cardiopulmonary arrest and died.
Discussion Questions
1. Summarize the patient history.
2. Summarize the available anesthesia data.
3. Summarize the postoperative laboratory studies.
4. Summarize the radiographic studies.
5. What main ethical issues define this case?
6. What scenario might have allowed for a different outcome postoperatively and what might that have looked like? What specific choices might the post-operative care team have made?
7. Patients move from one unit or care floor to another in hospitals. How, as a provider, would you ensure continuity of care? What provider issues may affect continuity? What system issues may affect continuity? What is the role of charting in ensuring continuity? What other factors facilitate patient care continuity inside a hospital?
Back to history
Case 9
(Click to view all parts)
Spleen dissection
Preview:
Case 9 – History 1
Brief History
[The patient was a middle-aged Caucasian woman. The purpose of this video is to show a spleen dissection from our archives.
There is only one video.]
Case 10
(Click to view all parts)
Post-colonoscopy complication
Preview:
Case 10 – History 1
Brief History
The patient was an elderly Caucasian man with history of chronic gastrointestinal bleeding (from a polyp) requiring periodic blood transfusion.
The patient underwent elective colonoscopy with polypectomy.
Due to post-procedural malaise and abdominal pain, a computed tomography scan was performed which showed free air in the abdomen.
The patient died several days later.
The history is obtained from the family.
Discussion Questions
1. Summarize the history.
2. What are complications of colonoscopy?
3. The patient had chronic gastrointestinal bleeding requiring periodic transfusions. What judgment and clinical data would factor into the decision to undergo a procedure vs. continue periodic transfusions?
4. The patient underwent a polypectomy. What judgement and clinical data would factor into the decision to perform a polypectomy vs. a biopsy during colonoscopy?
Back to history
Case 11
(Click to view all parts)
Gastrointestinal bleeding and sudden death
Preview:
Case 11 – History 1
Brief History
The patient was an elderly Caucasian woman with recent bleeding per rectum, anemia and unspecified cardiac arrhythmia.
She was hospitalized for her bleeding and received transfusions.
An endoscopy did not find the source of the bleeding.
Mobility at home was limited and she was scheduled for outpatient physical therapy.
On descending the stairs at home going to her first physical therapy appointment, she became short of breath.
She arrived at physical therapy where she collapsed and died.
The history is obtained from the family.
Discussion Questions
1. Summarize the history.
2. What is the differential diagnosis for bleeding per rectum?
3. In general, why might an endoscopy not find the source of bleeding?
4. What causes of death does the history suggest? Which is most likely?
Back to history
Case 12
(Click to view all parts)
Sudden death
Preview:
Case 12 – History 1
Brief History
The patient was an elderly Caucasian man with diabetes (poorly compliant with insulin regimen), hypertension, hypercholesterolemia, hydrocephalus, and remote and possibly recent strokes of unknown laterality.
The family reports the patient was more sedentary recently, noting a shuffling gait.
Last contact with the decedent was approximately one week prior.
He did not have complaints at that time.
He was found on the floor next to his bed and fecally incontinent after an unwitnessed cardiopulmonary arrest.
The family noted two days of unread mail.
This history is obtained from the family.
Discussion Questions
1. Summarize the history.
2. Discuss adult-onset hydrocephalus.
3. Create a differential diagnosis for the cause of death, based on the history.
Back to history
Case 13
(Click to view all parts)
Sudden death
Preview:
Case 13 – History 1
Brief History
The patient was an elderly Caucasian male with hypertension, insulin-dependent diabetes mellitus with history of diabetic comas and neuropathy, status post coronary artery bypass graft (CABG) surgery approximately 5 years prior, inability to walk, and multiple admissions to hospitals and rehabilitation centers over the past year for a variety of problems including dehydration, elevated ammonia, weight loss, congestive heart failure, food poisoning, pacemaker-defibrillator placement, deep right hip infection with MRSA, and increasing ascites.
The patient was in rehabilitation where he was found on the floor after an unwitnessed fall.
There was concern for bruising.
He died later that day.
The history is obtained from the family.
Discussion Questions
1. Summarize the history.
2. How would you characterize the severity of the patient’s diabetes?
3. What are the main, underlying medical problems of the patient?
4. Why might this patient have an elevated ammonia? What other part(s) of the history might support your answer?
5. What could cause a fall, such as this patient had?
6. When a patient dies after a fall, what might explain this?
7. What concerns might families have about an unwitnessed fall in a rehab setting?
8. What constitutes “appropriate monitoring” in a nursing home? In rehab? On a general medical floor? In the ICU?
9. How is trust built between providers and patients/families?
10. The family was concerned about bruising after the fall. In the setting of an unwitnessed fall, one family might attribute bruising to the fall. Another family might suspect foul play. How would you account for this difference in views? What can you do, as a provider, to build trust with a family?
Back to history
Case 14
(Click to view all parts)
Recent chest pain
Preview:
Case 14 – History 1
Brief History
The patient was a middle-aged Caucasian man with a history of hypertension who was seen recently for extensive cardiac workup after complaints of chest discomfort.
Work-up was negative.
He complained the night before death of some possible chest tightness.
He woke up in the morning, went to the bathroom, was observed to be short of breath and collapsed.
Paramedics were called.
The patient received advanced life support measures, including intubation, but died.
Discussion Questions
1. What’s the differential diagnosis for sudden onset of shortness of breath followed by collapse (see history)?
2. What’s the differential diagnosis of the patient’s collapse based on the complete history?
3. How do you interpret the negative work-up after presenting recently with chest pain?
4. You are the treating provider. Your patient presents with a complaint of chest tightness. What do you include in your work-up?
5. You are the treating provider. Your patient with chest tightness has a “negative” work-up. What next steps would you take?
Back to history
Case 15
(Click to view all parts)
Chronic pain and sudden death
Preview:
Case 15 – History 1
Brief Past Medical History
The patient was a middle-aged Caucasian man with chronic pain related to a work injury to the right wrist approximately 10 years prior.
A wrist surgery did not relieve his pain.
He was managed with multiple pain medications.
“Ganglion” injections of the neck also did not help his pain.
He complained of ongoing pain, was unable to work and became depressed.
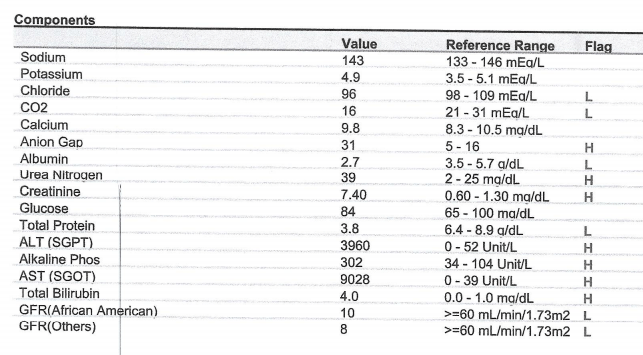
Case 15 – History 2
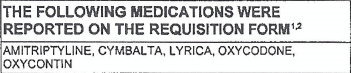
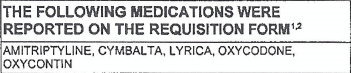
Premortem drug testing approximately 1 year prior to death
![]()
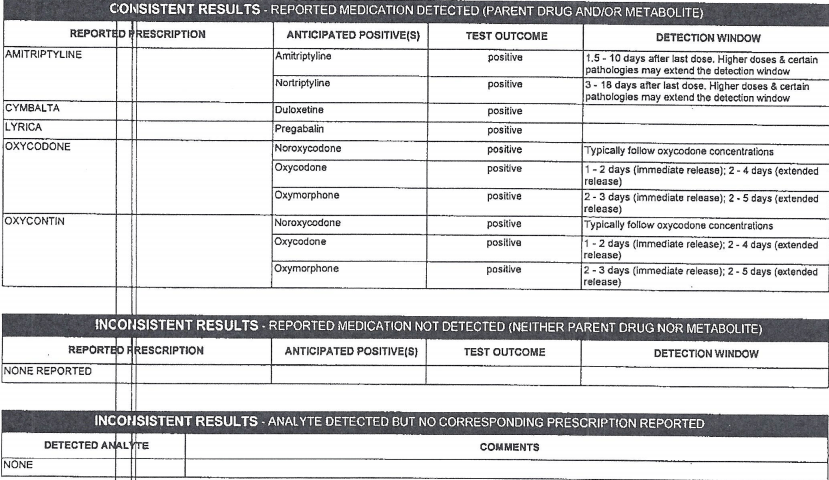
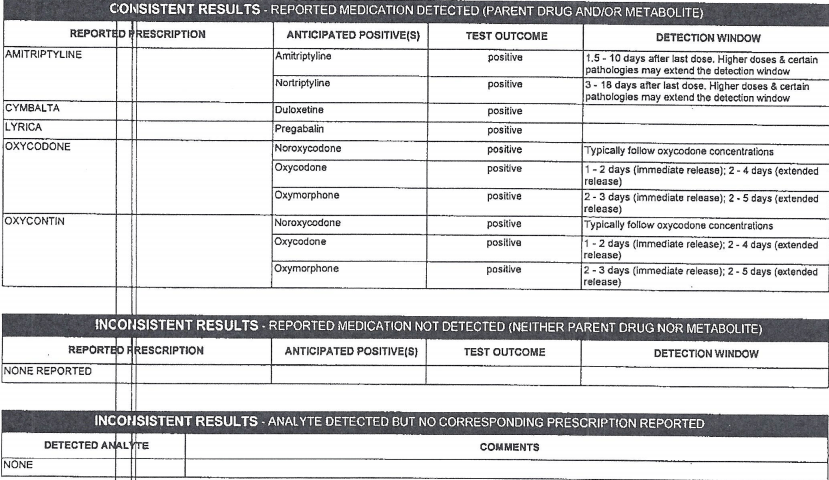
Part 2
![]()
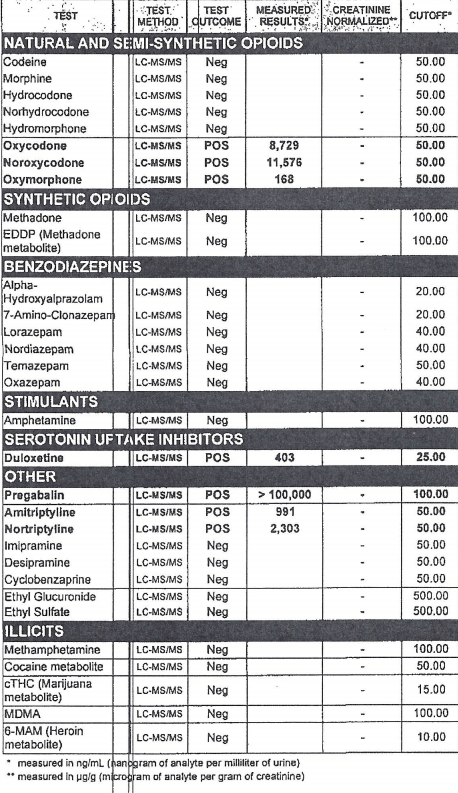
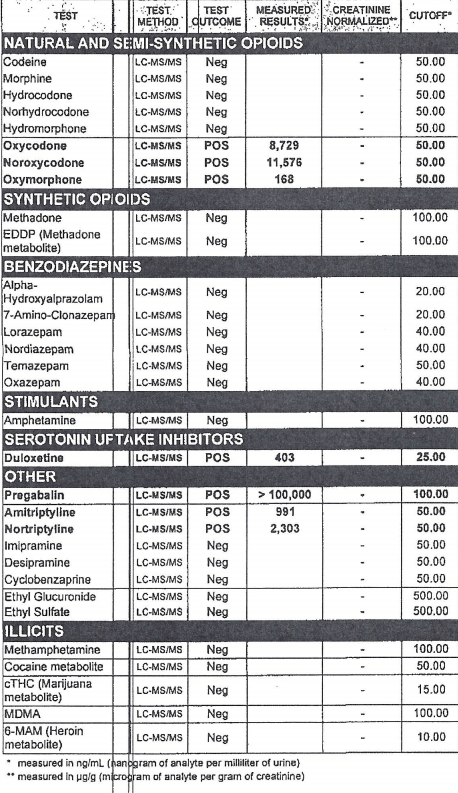
Part 3
![]()
Case 15 – History 3
Perimortem events
The patient died suddenly after an unwitnessed cardiopulmonary arrest.
The family states he did not take any pain medication on the day of death or the night before he died; but did take pain medication the morning of the day before death.
Discussion Questions
1. Summarize the history.
2. What type of fluid does the toxicology test?
3. Interpret the toxicology test. Would you make any changes or advisements to the patient as their clinician?
4. What is a differential diagnosis for why this patient might have died?
Back to history
Case 16
(Click to view all parts)
Dementia and kidney failure
Preview:
Case 16 – History 1
Brief History
The patient was an elderly Caucasian man, status post kidney transplant who had longstanding undiagnosed dementia.
Discussion Questions
1. What is likely the purpose of the brain removal in this case?
(See also questions for Case 5.)
Back to history
Case 17
(Click to view all parts)
Sudden death
Preview:
Case 17 – History 1
Brief History
The patient was a middle-aged Caucasian man with diabetes, high blood pressure, hypercholesterolemia, alcohol use disorder and poor self-care.
He underwent repeated debridement of a left foot ulcer recently.
He complained of continual “restless legs.”
The patient was found after an unwitnessed cardiopulmonary arrest.
Discussion Questions
1. Summarize the history and create a differential diagnosis for the cause of death.
2. What behaviors and physical exam findings might you expect in a patient with “poor self-care”?
Back to history
Case 18
(Click to view all parts)
Decomposition, history of clipped cerebral aneurysm
Preview:
Case 18 – History 1
Brief History
The patient was a middle-aged Latino man with history of clipped cerebral aneurysm approximately five years prior (presenting at that time with headache), obesity and recent dyspnea on exertion and recent headache.
The patient died suddenly after an unwitnessed cardiopulmonary arrest.
Discussion Questions
1. Summarize the history and make a differential diagnosis for the cause of death.
2. What is the differential diagnosis for headache?
3. How are cerebral aneurysms diagnosed?
4. How commonly are cerebral aneurysms multiple?
5. If the patient’s cerebral aneurysm surgery was five years prior, how likely is his recent headache related to the surgical site?
Back to history
Case 19
(Click to view all parts)
Hypertension, dizziness and sudden death
Preview:
Case 19 – History 1
Brief History
The patient was a middle-aged Caucasian woman with history of knee surgery and recent dizziness (typically while standing from bending over position) and difficulty walking.
The patient’s mother had a history of multiple malignancies, including a left frontal meningioma and lung cancer.
The patient died suddenly.
Discussion Questions
1. Summarize the history and create a differential diagnosis for the cause of death.
2. When is a family history of cancer more likely “sporadic” and when is it concerning for inherited or familial cancer?
3. What are some examples of inherited or familial cancers?
Back to history
Case 20
(Click to view all parts)
Elderly man with stroke
Preview:
Case 20 – History 1
Brief History
The patient was an elderly Latino man with stroke four months prior, recently admitted to rehab where he developed difficulty breathing.
This resolved, but there was concern for poor care, with decreased feeding as well as possible aspiration.
A nasogastric tube was ultimately inserted.
However, the tube was placed with difficulty requiring four attempts and concern for traumatic placement.
The patient subsequently decompensated.
He was admitted to hospice, put on comfort medication and died the following day.
Discussion Questions
1. Summarize the history.
2. What are complications of nasogastric tube placement?
3. Based on the history, what concerns were there about the patient’s care in rehab?
4. When is decreased feeding and aspiration more related to the patient’s condition (e.g., stroke)? When is decreased feeding and aspiration more related to care? In any given case, how could you tell?
Back to history
Case 21
(Click to view all parts)
History of breast cancer and alcohol use
Preview:
Case 21 – History 1
Brief History
The patient was a middle-aged Caucasian woman status post left breast lumpectomy and radiation therapy for ductal carcinoma in situ three years prior with follow-up maintenance chemotherapy regimen; hypertension; and alcohol use disorder.
There was a change in medication approximately 2 months prior due to symptoms of abdominal pain and weight loss.
Once the medication was stopped, her symptoms resolved; however, the patient was noted to have 40 lb. weight loss overall prior to death.
The patient was normally functioning the night before her death and was found unresponsive in bed by her boyfriend after an unwitnessed cardiopulmonary arrest.
Discussion Questions
1. Summarize the history.
2. What is the differential diagnosis of 40 lb. weight loss?
3. Why might this patient have died, based on the history?
Back to history
Case 22
(Click to view all parts)
Middle aged woman with psychiatric history
Preview:
Case 22 – History 1
Brief History
The patient was a middle-aged African American woman with history of psychiatric condition, obesity and recent weight loss.
The patient was transferred from her long-term residence to a hospital after an unspecified event in which she was found facedown.
Admission work-up included evaluation for a possible, unspecified respiratory issue.
She received medical management and was transferred to a rehabilitation center for possible, unspecified wound management.
The patient died under unknown circumstance in the rehabilitation center.
Limited history was available.
Discussion Questions
1. Summarize the history.
2. The history is limited. If you were seeing the patient in the emergency room, brought in by paramedics, what initial work-up would you order? Why?
Back to history
Case 23
(Click to view all parts)
Recent laparoscopic surgery
Preview:
Case 23 – History 1
Brief History
The patient was a middle-aged woman status post gastric bypass surgery (a Roux-en-Y procedure).
The post-operative course was complicated by abdominal discomfort.
The patient died suddenly.
Discussion Questions
1. How is laparoscopic Roux-en-Y performed?
2. Based on the history, what might be some possible causes of death?
Back to history
Case 24
(Click to view all parts)
History of coronary artery bypass graft and recent back surgery
Preview:
Case 24 – History 1
Brief History
The patient was an elderly Latino man with a history of four-vessel coronary artery bypass (remote), insulin-requiring diabetes, and liver transplant (remote).
He was in his usual state of health and working until approximately one year ago when he had back pain requiring surgery.
The subsequent year was marked by concern for dementia, 70 lb. weight loss and admission to a nursing home.
The patient had a witnessed sudden cardiopulmonary arrest and died.
Discussion Questions
1. Summarize the history.
2. What are the short and long-term complications of coronary artery bypass graft surgery. Which have an anatomic basis and what is the change that occurs? Which are related to the body’s natural reaction to the surgery? Which may be related to the operative procedure? Which may be related to the patient’s self-care choices?
Back to history
Case 25
(Click to view all parts)
Motor vehicle accident and untreated hypertension
Preview:
Case 25 – History 1
Brief History
The patient was a middle-aged man with hypertension reportedly up to systolic 170 (diastolic unknown) who took a hypertensive medication but discontinued recently and was trying natural methods of blood pressure control.
The patient was reportedly an experienced driver who used alcohol responsibly.
He was riding his motorcycle, fell off and crashed at approximately 20 miles per hour (witnessed event) and was unresponsive when the paramedics arrived.
Resuscitative measures were taken but the patient died at the scene.
A brother died from a stroke in his 50’s.
Discussion Questions
1. How do you understand the history?
2. Arriving at the scene, what questions do you have?
3. Why do people die in motor vehicle accidents? What is the likely cause of death here? (Revisit this question after viewing the physical exam, and then, after viewing each part of the case. Does your answer change? Why? What evidence has supported or changed your thinking?)
Back to history
Case 26
(Click to view all parts)
Dementia and nursing home fall
Preview:
Case 26 – History 1
Brief History
The patient was an elderly Caucasian woman, nursing home resident with dementia who fell approximately one week prior to death.
She sustained right facial and other right-sided injuries and was managed with pain medication.
She died suddenly after a large bowel movement.
Discussion Questions
1. How would you tell the difference between abuse and neglect in an elderly patient? What are signs of neglect in an elderly patient? What are signs of abuse?
2. If a patient has signs of neglect but not abuse, can this still be abuse? Why or why not?
3. The history describes a fall. In general, what patterns of injury would support that story? What patterns of injury go along more with abuse?
4. If the family tells you the patient was unable to walk and was bedridden, how does that change your understanding of the case?
5. If the family tells you the patient was ambulatory, how does that change your understanding of the case?
6. If the patient was verbal before the fall and non-verbal after, what’s your differential diagnosis?
Back to history
Case 27
(Click to view all parts)
Dialysis
Preview:
Case 27 – History 1
Past Medical History
The patient was a young African American woman with congenital, familial kidney disease requiring dialysis, status post two shunts (including a HeRO graft) and an arterio-venous fistula in the left arm.
Each of these clotted.
When second shunt in the arm clotted, a temporary intravenous vascular site was inserted into the right neck prior to a new (third) shunt being placed in the left thigh.
This third shunt remained patent and functional.
The patient’s course was also complicated by pulmonary embolism (suspect origin: the clotted HeRO graft).
For her pulmonary embolism, the patient was started on Coumadin and home oxygen.
There was consideration of operative removal of clots.
For unknown reasons, the patient’s Coumadin was discontinued approximately 6 months after the onset of the pulmonary embolism.
Case 27 – History 2
Day of death
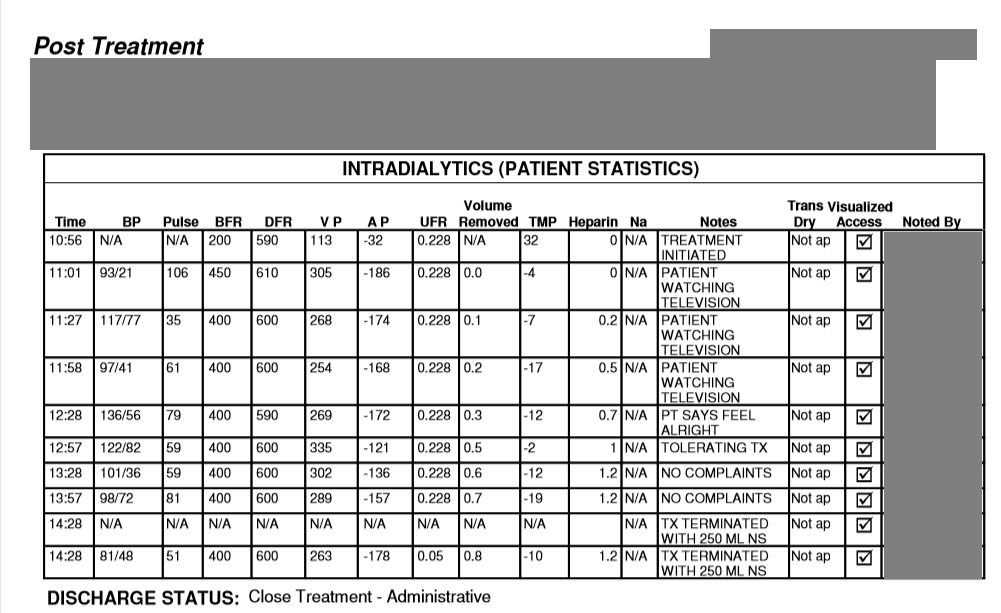
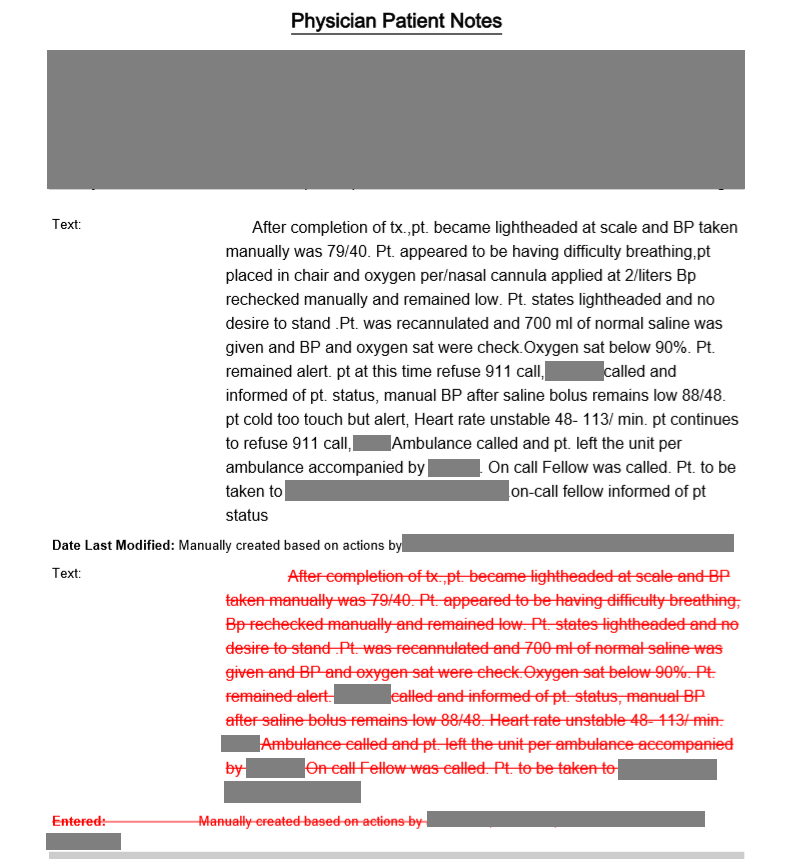
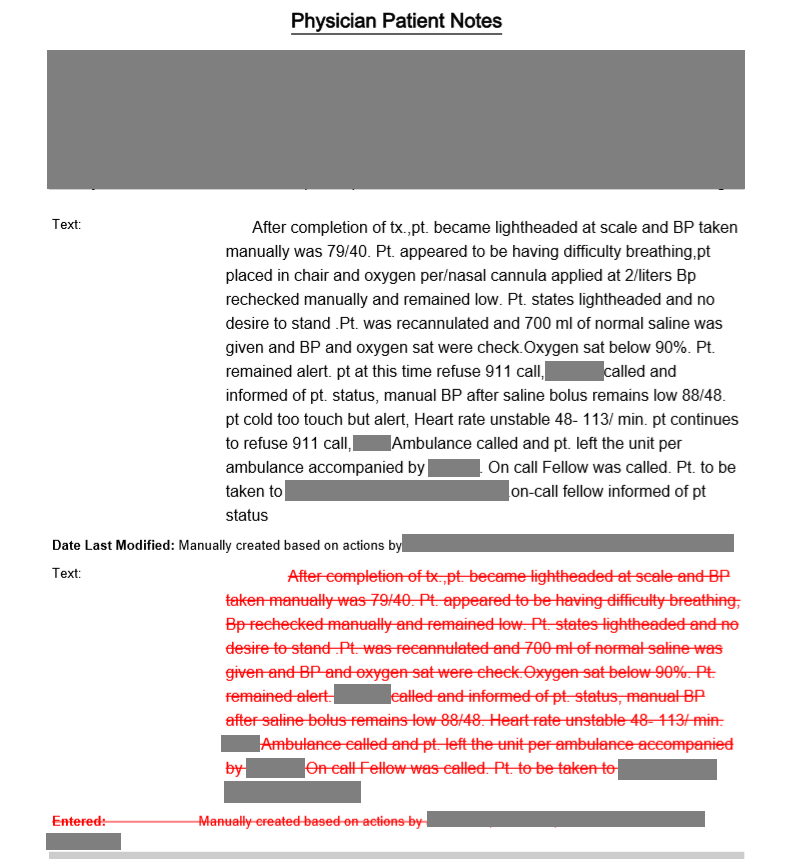
Approximately two months after Coumadin was discontinued, the patient became hypotensive and short of breath at the end of a dialysis session.
Case 27 – History 3
Partial dialysis records – day of death
![]()
Case 27 – History 4
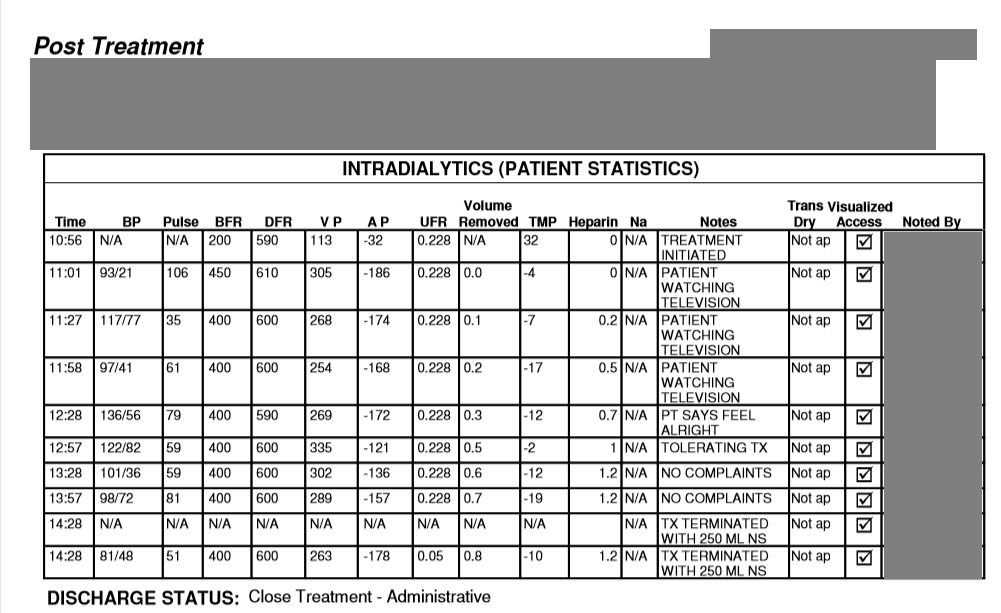
Dialysis Clinic Notes – day of death
![]()
Case 27 – History 5
Emergency Services Trip Record – day of death
![]()
Case 27 – History 8
Death
The patient died despite resuscitative efforts.
Discussion Questions
1. Summarize the history.
2. Based on the dialysis record, why was dialysis terminated early?
3. Review the records and decide how much time elapsed between the end of dialysis and the time the paramedics were called? What explains this? Is there a concern?
4. Whose responsibility is it to call 911 in a dialysis center or any outpatient or medical facility? What if the patient does not want 911 called? What is the right decision?
5. What is the difference between the initial Clinic Notes and the revised Clinic Notes from the dialysis center on the day of death? Why do you think these changes were made?
6. How does the Emergency Services Trip Record contribute your understanding of the events?
7. What would you have done differently in the dialysis center?
8. What ethical issues does this case present?
9. What’s the difference between a dialysis shunt, graft and fistula?
10. What are common complications of each?
11. This patient had three operations for dialysis access. Each clotted and stopped working. How might this relate to the patient’s clinical history?
12. What is a HeRO graft?
13. What are some common causes of kidney failure?
14. What emergencies can be associated with kidney failure?
15. What emergencies can be associated with dialysis?
Back to history
Case 28
(Click to view all parts)
Peripheral vascular disease and recent angioplasty
Preview:
Case 28 – History 1
Brief History of Present Illness
The patient was a middle-aged Latina woman with history of right lower leg pain she initially thought was an insect bite.
Case 28 – History 2
Initial assessment
On presenting for medical care, she was found have to peripheral vascular disease.
Case 28 – History 3
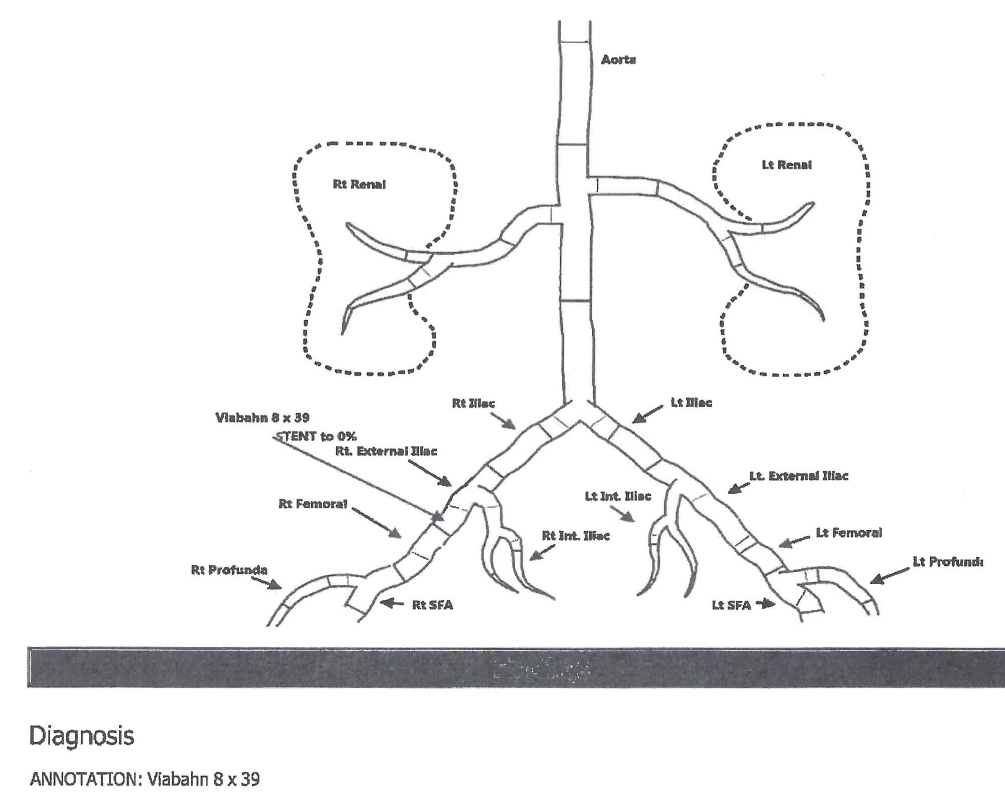
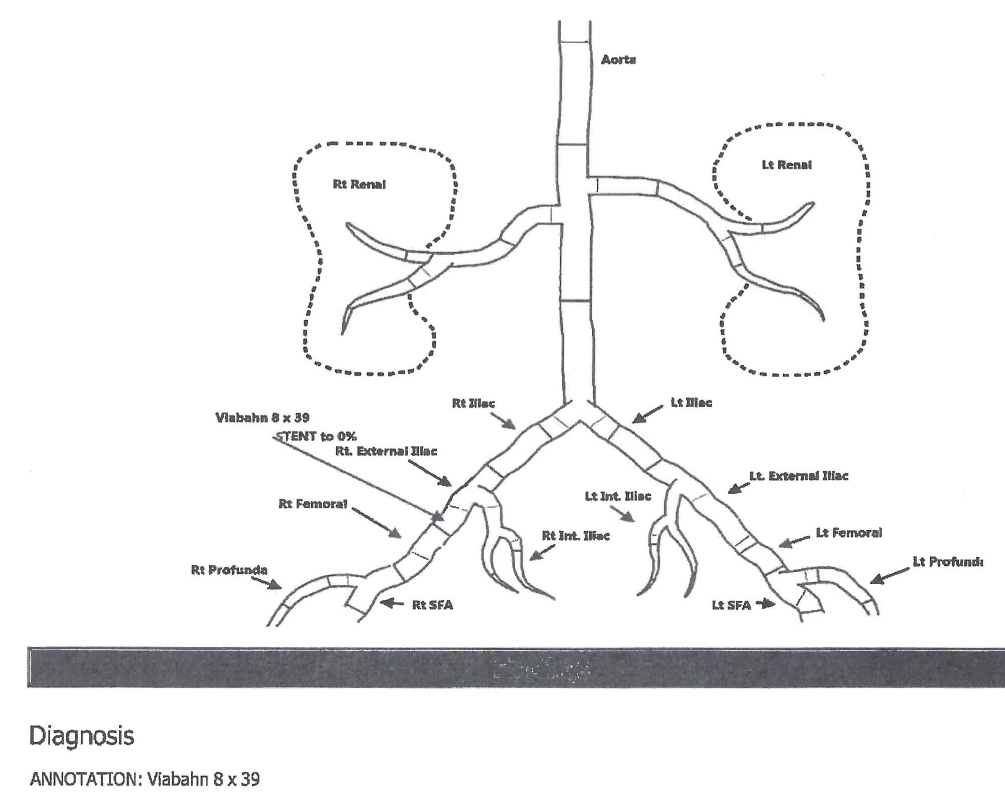
Initial (Pre-operative) Angiogram
Pre-operative Echocardiogram
Case – History
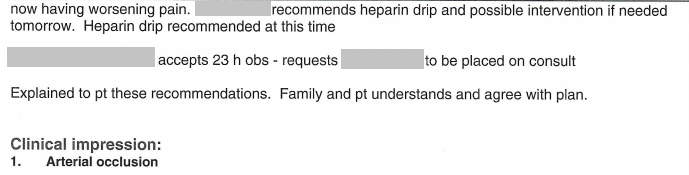
Hospital course
She underwent an emergency thromboembolectomy of the right femoral, popliteal, anterior tibial and right tibioperoneal trunk arteries; and patch angioplasty of the right popliteal artery.
The pain was mildly improved after the procedure.
Five days postoperatively, she developed blisters and pain at the surgical site and was diagnosed with reperfusion syndrome.
After a number of days, she was discharged home still in considerable pain.
Case 28 – History 4
Second admission
She returned to the emergency room approximately 2 week later in severe, intolerable pain localized to the right lower leg and was admitted.
Case 28 – History 5
Right lower extremity arterial duplex ultrasaound report – second admission
Part 1
![]()
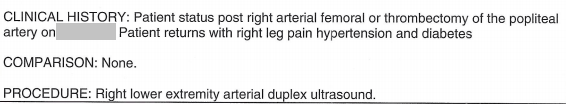
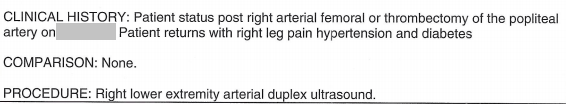
Part 2
![]()
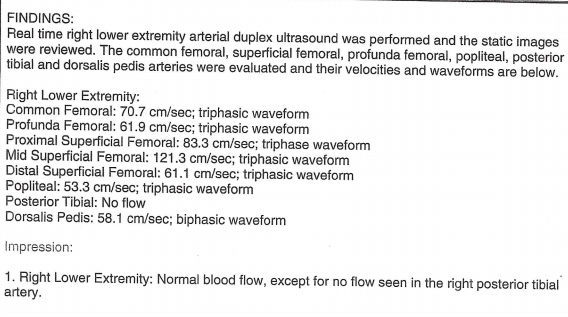
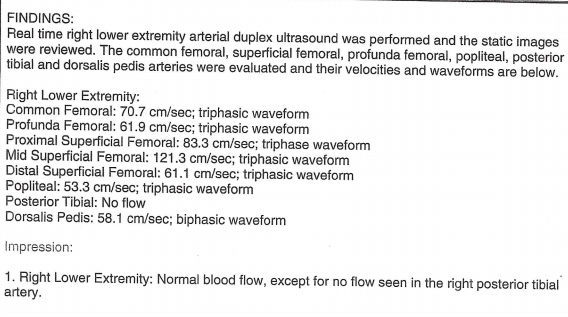
Case 28 – History 6
Emergency room physician note – second admission
Part 1
![]()
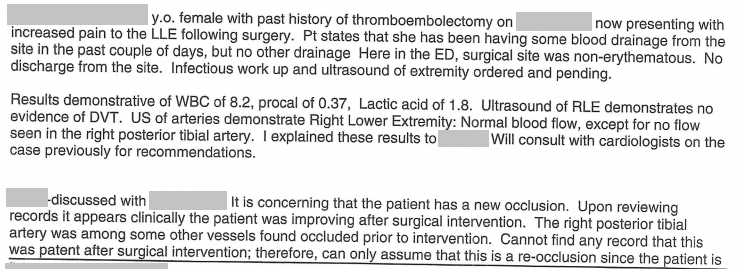
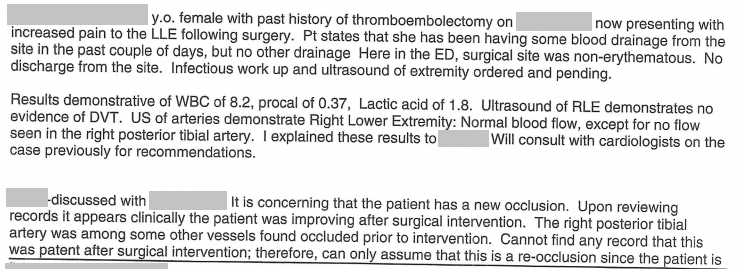
Part 2
![]()
Case 28 – History 7
Hospital course – second admission
On admission, she was tachycardic.
The patient had a second vascular procedure of the right leg (atherectomy of right posterior tibial artery and balloon angioplasty of right anterior tibial artery).
Case 28 – History 8
Intraoperative angiogram – second surgery
Case 28 – History 9
Intraoperative vital signs – second surgery
![]()
Case 28 – History 10
Additional hospital course – second admission
Within several days post-operatively, she developed shortness of breath and died.
Discussion Questions
1. Summarize the history.
2. Review the initial angiogram. What vascular structures can you identify? Which are patent? Which are occluded. Construct a diagram to show which arteries are patent, which are occluded, and by how much.
3. Review and assess the preoperative echocardiogram.
4. The history indicates three major decisions: the first operation, the hospital discharge, and the second operation. Evaluate each based on the clinical data. Which decisions do you agree with? What would you do differently? What additional information might be helpful?
5. If you had chosen to discharge the patient after the first operation, what would your discharge instructions have looked like?
6. What are the systemic consequences of ongoing pain? Did the patient manifest any of these?
7. Review the emergency room studies and emergency room physician note. What did the venous doppler find? What did the arterial study find? How did the arterial study compare to any prior studies according to the physician note?
8. Evaluate the emergency room physician’s logic in determining the cause of the patient’s pain. Do you agree? Come back to this question after viewing all the videos. Has your assessment changed? If so, why?
9. The emergency room physician documents the word “presume” in the medical record. When is this kind of thinking acceptable in clinical care? Can you give an example of when it is? When it is not? When is it dangerous to make presumptions or assumptions in medicine? Is it ever safe to make a presumption or assumption in medicine? Come back to this question after viewing all the videos. Have your answers changed? If so, why?
10. Even if you do not agree that it is acceptable to make a presumption, does the data support the kind of presumption the physician made? Why or why not?
11. You are the provider. Your patient’s condition worsens, yet available studies remain unchanged. How do you interpret this? How will you proceed? What resources can you draw on? (Revisit this question after studying the case videos.)
12. What are some likely reasons this patient could have died?
13. Come back to the history after viewing all the parts of the case. Reassess the clinical data in light of what you know about the patient’s anatomy and condition. Do you think there were any medical errors? If so, what were they? What data could you review to support your thinking? Do you think there was one error by one person? Or multiple errors by multiple people? Was this a diagnostically difficult case? Or were the errors more easily avoidable? What training issues present here?
14. What is your attitude towards medical errors? Does it depend on the type of error? The outcome? If you think there were errors in this case, what types of errors were there? Is one type more “correctable or preventable” than another? Which could be addressed systemically? Intradepartmentally? Individually?
Back to history
Case 29
(Click to view all parts)
Leg swelling
Preview:
Case 29 – History 1
Brief History
The patient was a middle-aged Caucasian woman who had a respiratory infection approximately one month prior, during which time she developed left leg swelling.
The patient died suddenly after an unwitnessed cardiopulmonary arrest.
Discussion Questions
1. What is the differential diagnosis for unilateral leg swelling? How would you distinguish one from another?
2. What is the differential diagnosis of bilateral leg swelling? How would you distinguish one from another?
3. Based on history, why do think the patient might have died?
Back to history
Case 30
(Click to view all parts)
Alcohol use disorder and patellar tendon repair
Preview:
Case 30 – History 1
Brief History
The patient was a middle-aged Caucasian man with alcohol use disorder, atrial fibrillation, hypertension, status post coronary artery bypass surgery, pulmonary fibrosis (unknown etiology), cataract surgery complicated by detached retinas, arthritis, a skin condition with “fistulas,” and status post double knee replacement five years prior.
Six weeks before death, he accidentally tore his left patellar tendon which was surgically repaired.
The post-operative course was complicated by left foot ulceration and superior migration of the patella.
The patient went for a post-operative clinic visit and was later that day found dead after an unwitnessed cardiopulmonary arrest.
Discussion Questions
1. Summarize the history and clinical issues.
2. Why do you think the patient might have died?
Back to history
Case 31
(Click to view all parts)
Young male.
Second autopsy.
Preview:
Case 31 – History <1/p>
Brief History
This was a second autopsy on a young African American man without prior medical issues.
Discussion Questions
1. What are some reasons a family might request a second autopsy?
2. Why do you think we can’t disclose much history?
Back to history
Case 32
(Click to view all parts)
Elderly woman with dementia and post-operative lethargy
Preview:
Case 32 – History 1
Brief History
The patient was an elderly Caucasian woman with Alzheimer’s disease, status post abdominal hernia repair (remote), who underwent knee replacement surgery approximately one month prior.
The family noted worsening mental status in the perioperative period.
The patent was admitted to a nursing care facility.
Over the next couple weeks, she was found difficult to rouse and had a witnessed cardiopulmonary arrest at the nursing facility.
CPR was performed but the patient could not be revived.
The family notes new administration of centrally acting agents during this time.
The autopsy was performed three days after death.
Whole blood postmortem toxicology showed ethyl alcohol, 0.049 gm/dl and lorazepam, 15.2 ng/ml.
Discussion Questions
1. Summarize the history and clinical issues.
2. Why do you think the patient might have died?
3. What is the differential diagnosis of post-operative mental status change?
4. What is the differential diagnosis of post-operative somnolence?
5. Can you suggest a plausible explanation of the symptoms and cause of death that had nothing to do with medication administration?
6. Could the symptoms and death have been related to medication administration? Why or why not?
7. Families may or may not have a realistic understanding of clinical issues. What factors go into a family’s understanding of their loved one’s medical issues? What steps can you take, as a provider, to assist with a family’s understanding?
8. You are the patient’s provider. You do not believe the patient died from drug effect, although you are not sure exactly why the patient was somnolent. The family meets with you and insists the somnolence and death were from the medication. How will you respond?
Back to history
Case 33
(Click to view all parts)
Middle-aged man with hypertension and chest pain
Preview:
Case – History
Brief History
The patient was a middle-aged Caucasian man with hypertension and history of cardiac ablation one year prior for unspecified arrhythmia.
He experienced the sudden onset of chest pain, presented to the emergency room and died eight hours later.
The patient was HIV negative.
Discussion Questions
1. Summarize the history and clinical issues.
2. You are an emergency room provider. How might your care differ, if at all, knowing the patient had a prior cardiac ablation (vs. not knowing this information)?
Back to history
Case 34
(Click to view all parts)
Shortness of breath in an elderly woman with COPD and obesity
Preview:
Case – History
Brief History of Present Illness
The patient was an obese, elderly Caucasian woman with history of hypertension, diabetes, atrial fibrillation (on Coumadin), COPD, asthmas, and May Thurner syndrome (status post recent stent placement in the left iliac vein), who presented to the emergency room after waking up in the middle of the night with shortness of breath.
This was not relieved by multiple nebulizer treatments at home.
She could not lie flat because she felt “breathless.”
She also complained of left-sided chest plain.
There was no fever or upper respiratory symptoms.
Case – History
Hospital course
On admission, Troponin I, POC was 3.18 ng/mL and BNP was 754.9 pg/mL.
She was diagnosed with a non-ST elevation myocardial infarction and treated with IV heparin and beta blockers.
On hospital day 2, Troponin I levels were 3.85 and 3.02 ng/mL.
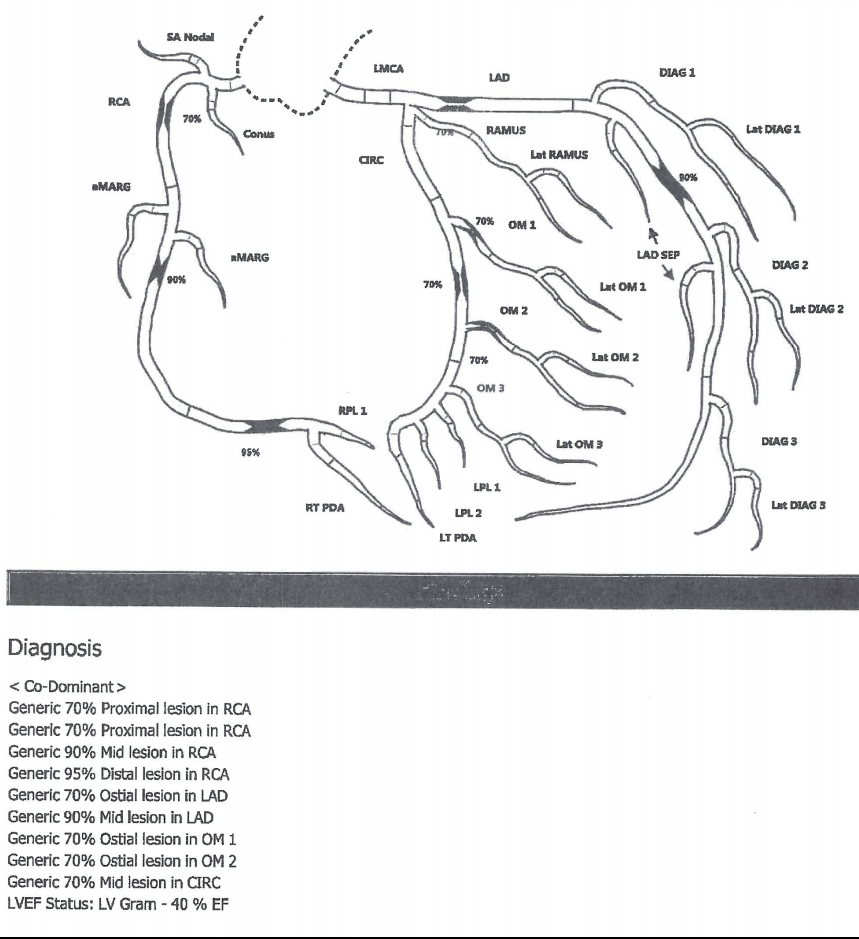
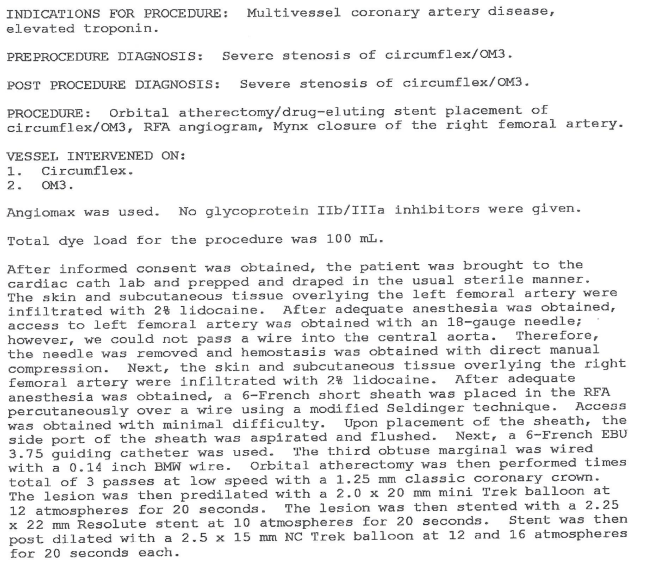
Case – History
First cardiac catheterization
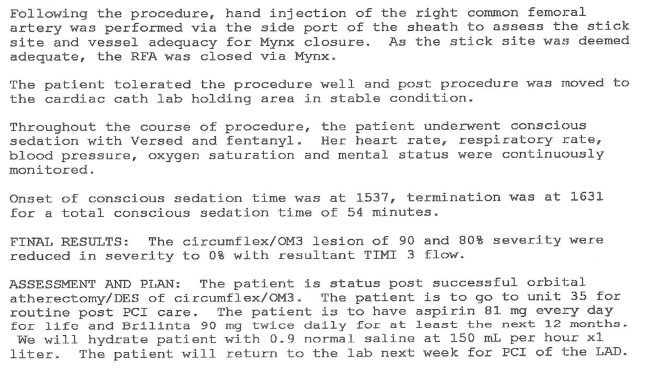
On hospital day 3, the patient underwent a cardiac catheterization.
Case – History
Left heart catheterization procedure note and diagram
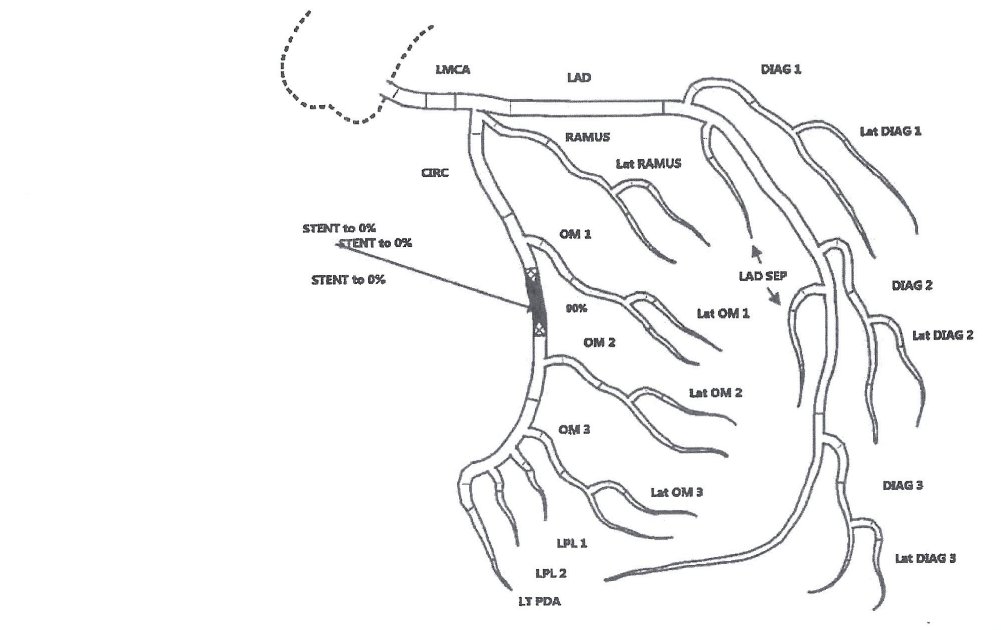
Page 1
![]()
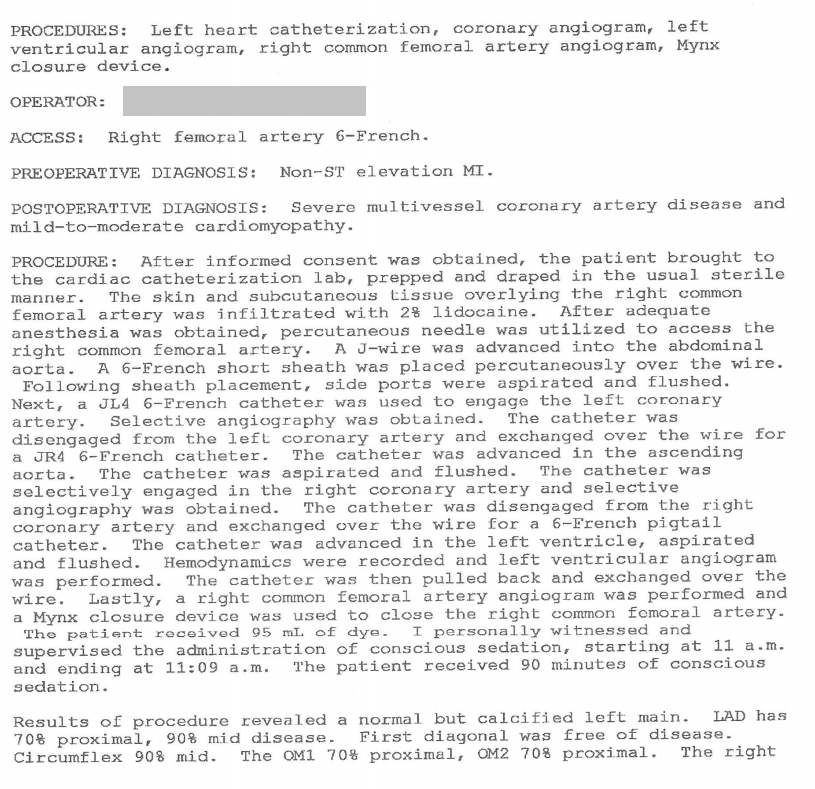
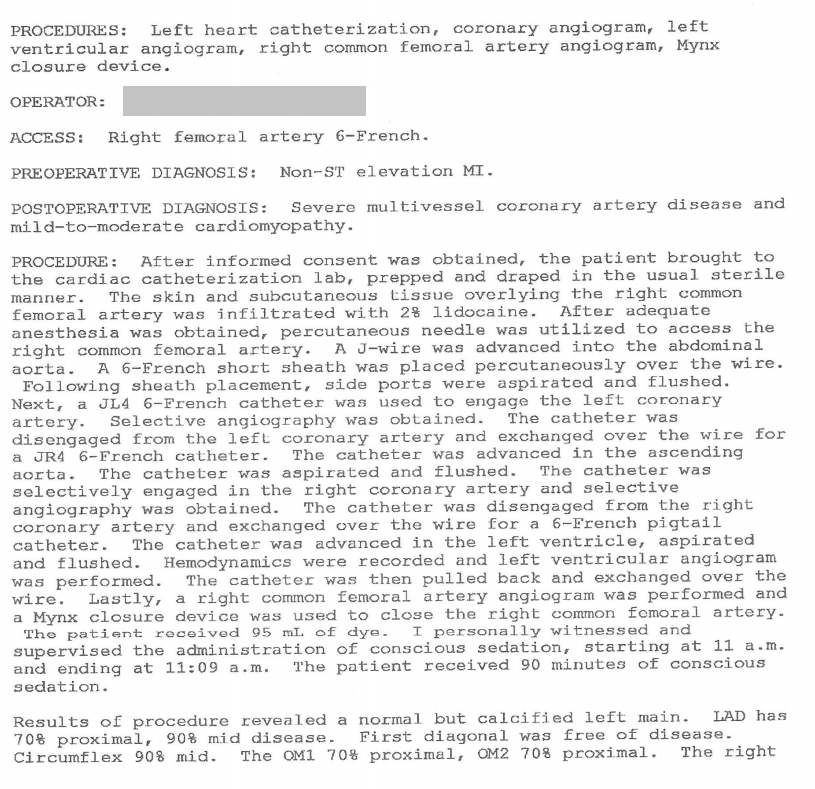
Page 2
![]()
Diagram
![]()
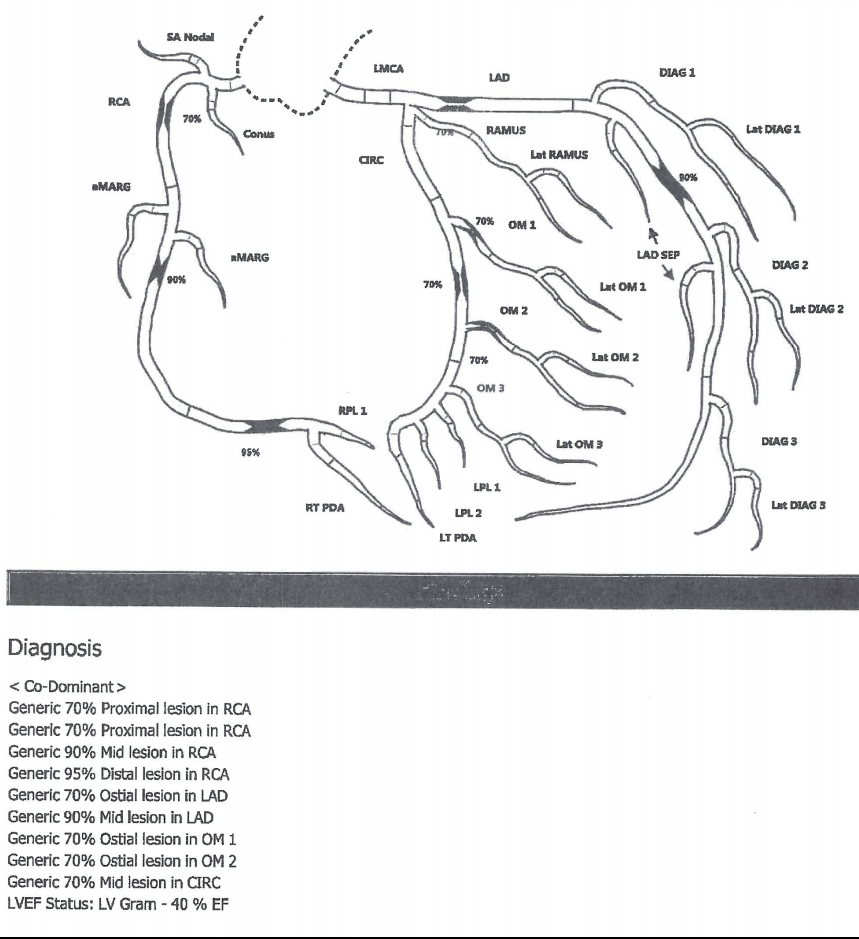
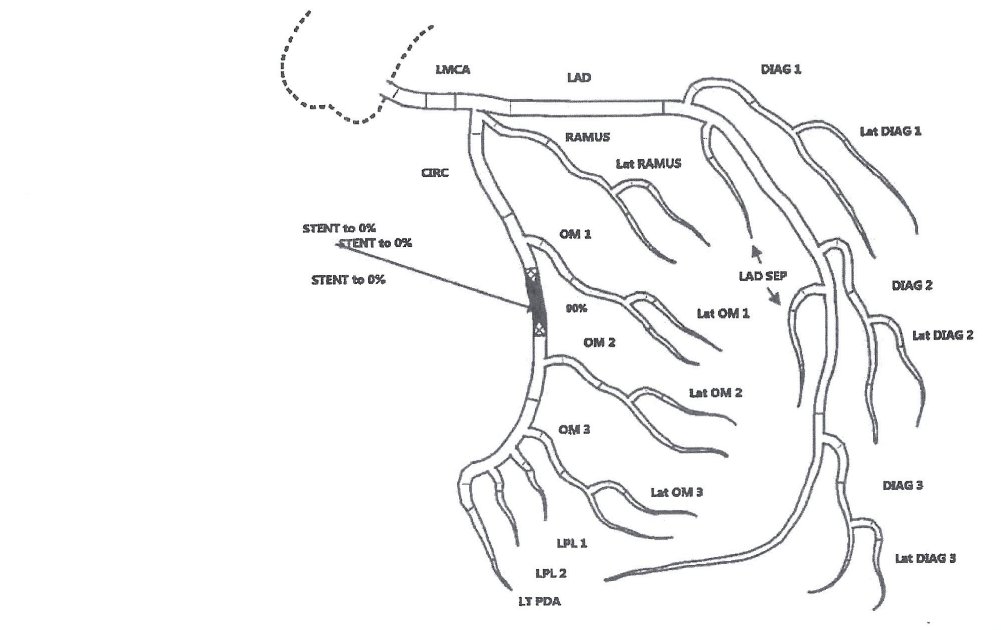
Case – History
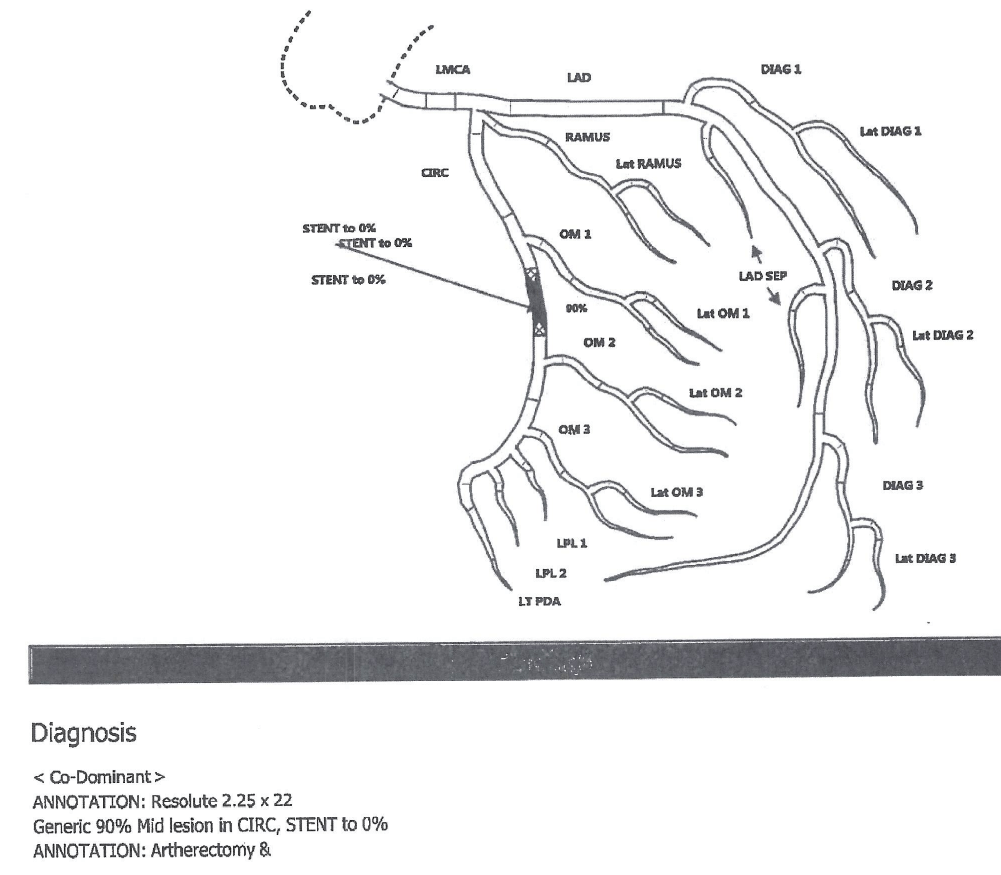
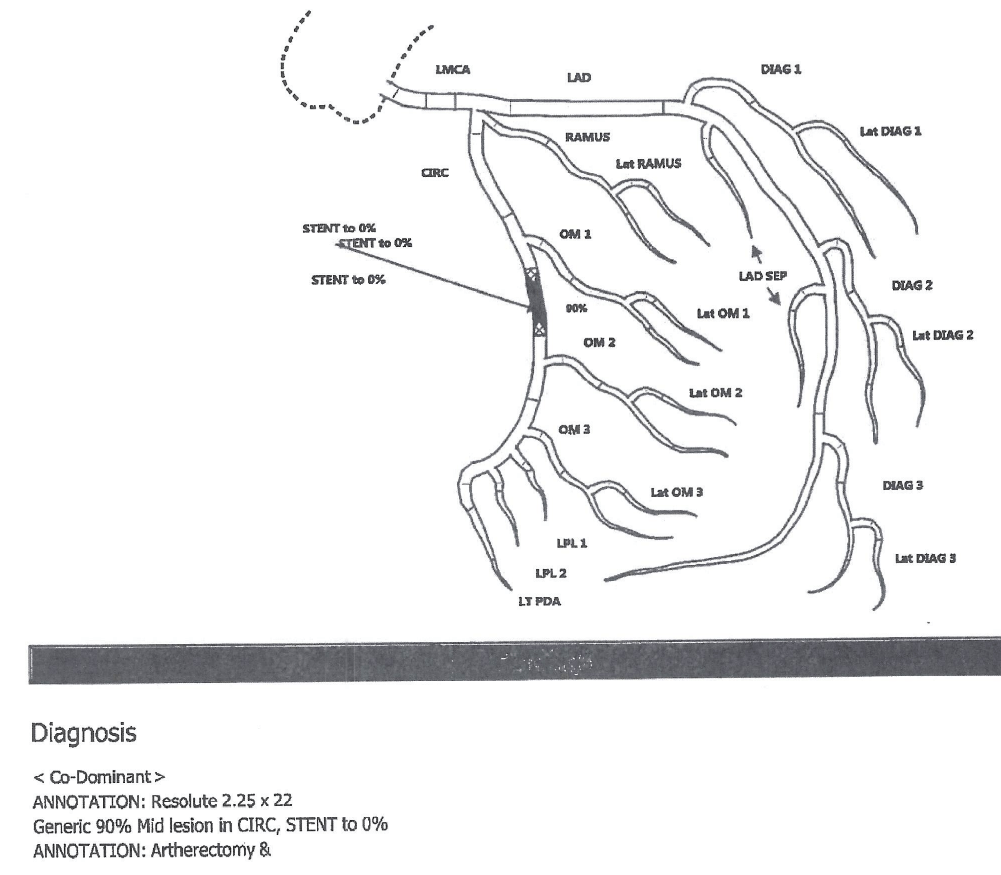
Second cardiac catheterization
She was deemed not a candidate for bypass surgery (due to her lung condition) and instead underwent coronary stent placement (hospital day 5).
Case – History
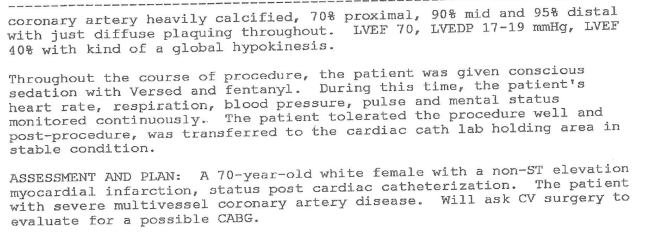
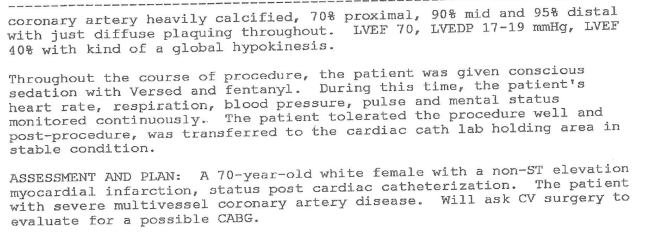
Second left heart catheterization (with stent placement) procedure note and diagram
Page 1
![]()
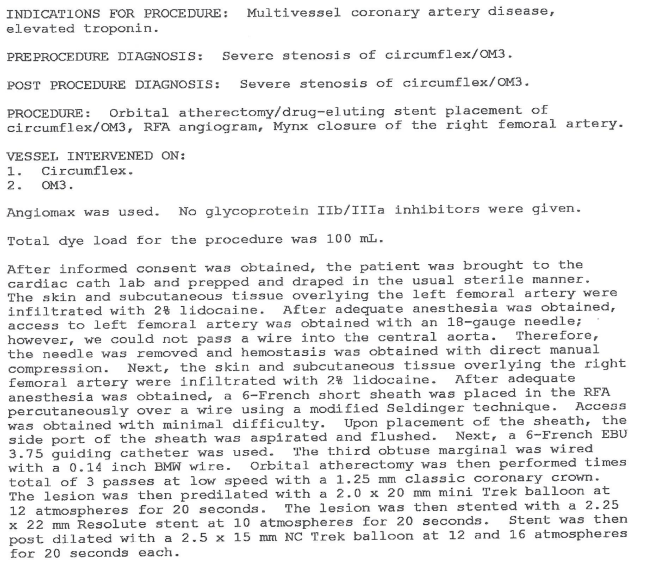
Page 2
![]()
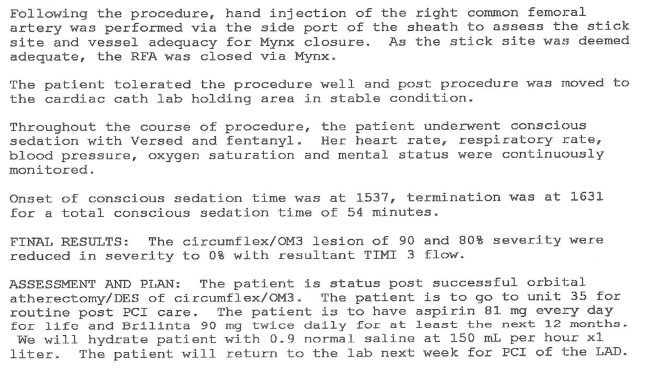
Diagram
![]()
Case – History
Immediate post-catheterization
The patient was stable in the immediate post-operative period
Case – History
Later in the day
Later that day, the nurse was unable to find a pulse in the right foot.
The patient was agitated with some mental status changes.
She notified the physician of both issues.
Case – History
Physician assessment
The physician found the patient to be tachypneic and short of breath, with no pulse on the right foot by doppler and also complaining of groin pain.
The patient was saturating 82% on room air.
He noted a possible right groin hematoma.
An ultrasound was to be ordered to rule out hematoma, per the physician note.
The patient was placed on a nonrebreather mask with improved oxygen saturation to 99% by arterial blood gas.
The patient’s tachypnea was attributed to anxiety and the patient was prescribed Ativan.
Case – History
Overnight
Throughout the evening and overnight the patient remained somewhat confused.
Case – History
The following morning
In the morning (hospital day 6) the patient was found hypotensive with a rigid abdomen.
She was intubated emergently.
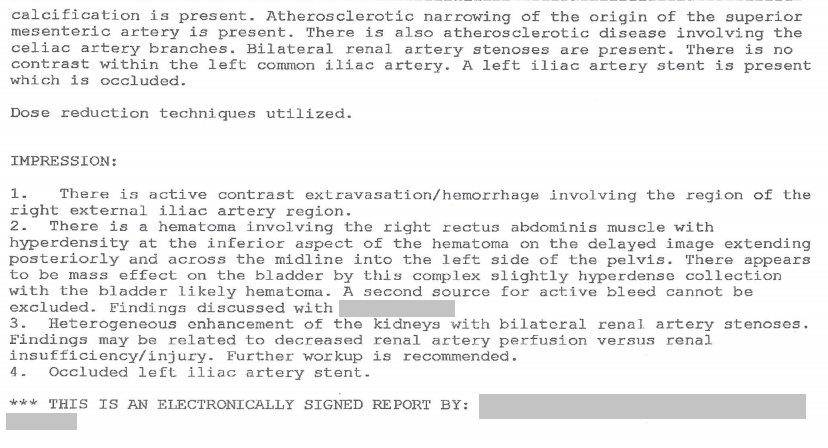
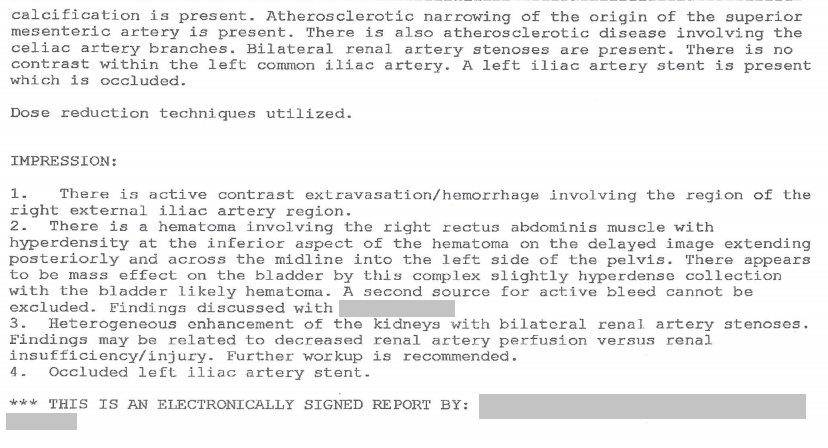
The patient had a CT of the abdomen and pelvis with contrast.
There is no record of an ultrasound being performed by this time.
Case – History
Results of CT Abdomen and Pelvis
Page 1
![]()
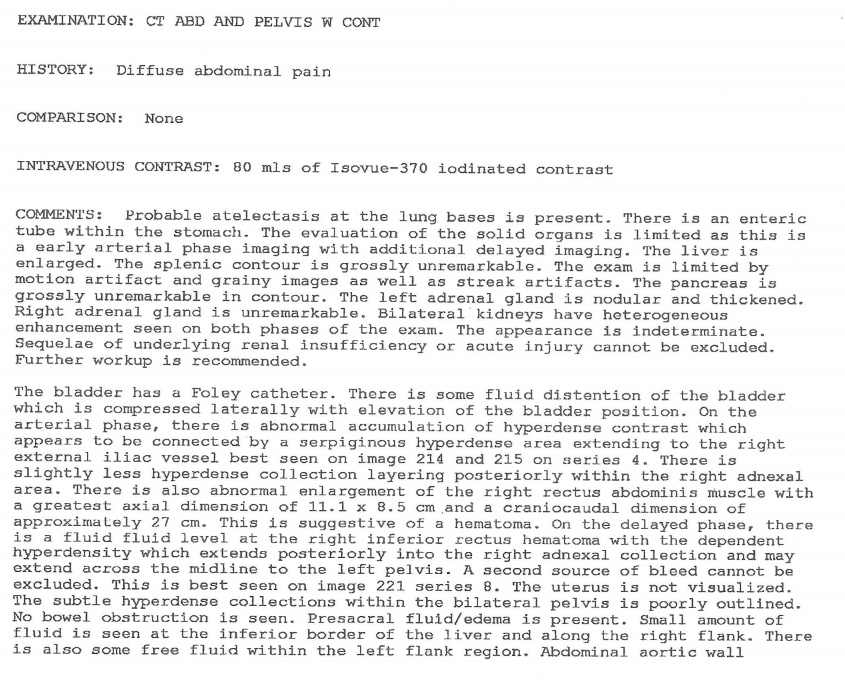
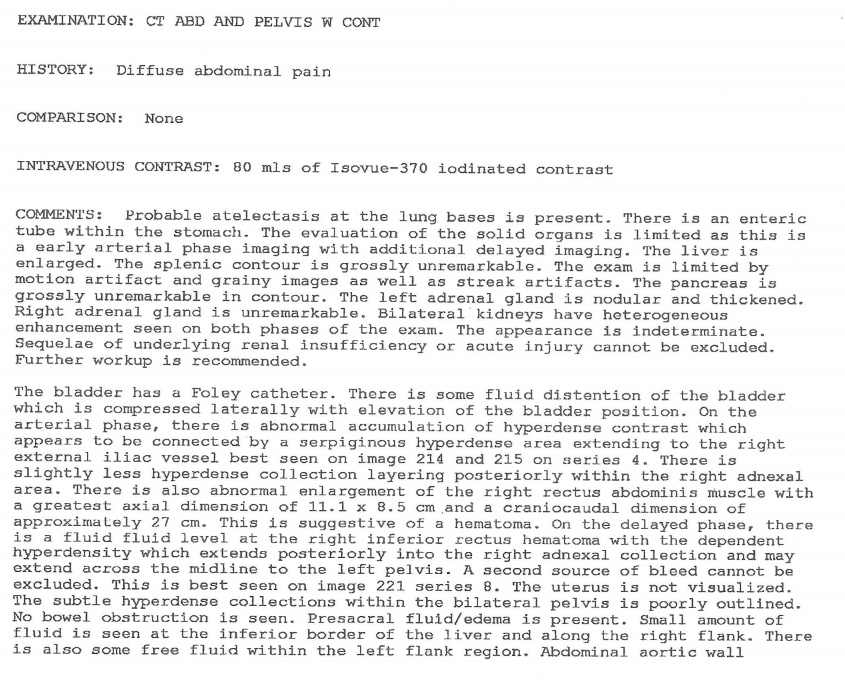
Page 2
![]()
Case – History
Placement of stent/patch
The patient underwent abdominal aortography with placement of a patch.
Case – History
Abdominal aortography procedure note and diagram
Page 1
![]()
Page 2
![]()
Diagram
![]()
Case – History
Hospital course (continued)
The patient could not be stabilized, required 10-15 units of blood over the next several hours and died.
Discussion Questions
1. Summarize the history.
2. What is the differential diagnosis of sudden onset of shortness of breath in the patient with obesity and COPD?
3. How many cardiac catheterizations did the patient have?
4. How does a cardiac cath work?
5. What is a coronary stent?
6. What medical conditions are associated with obesity?
7. What steps would you take to safely lift, turn, or transport a patient of this size?
8. What surgical risks increase for obese patients?
9. How much more difficult is it to insert a catheter into the groin of an obese patient than a thin patient?
10. What key medical errors were made in this case? What would you have done differently? (Revisit this question after viewing the entire case. Did your answer change? If so, why?)
11. The nurse diligently reported a key postoperative clinical finding to the physician. What was that key finding?
12. After learning a key postoperative clinical finding, the physician made an assessment that did not address a life-threatening issue. Why do you think this happened? What internal, relationship, or training factors might explain this outcome? How might this be addressed with this physician?
13. When does the nurse’s role extend beyond reporting of critical information? What is the nurse’s role when the physician makes a determination that puts the patient at risk? What is a team’s role when a key member makes an error, does not address issues competently, or puts a patient’s life at risk?
Back to history
Case 35
(Click to view all parts)
Motor vehicle accident
Preview:
Case – History
Brief History
The patient was a pre-adolescent African American elementary school student.
He was in the back seat of a car during a single vehicle accident into a stationary object.
The paramedics arrived.
The patient was transferred to a local hospital where he received resuscitative efforts for an hour but died.
The other passengers, including the driver, received unspecified injuries requiring hospitalization but survived.
No adults were in the vehicle at the time of the accident and the driver was not licensed.
Discussion Questions
1. Summarize the history.
2. What are your objectives upon arriving at the scene?
Back to history
Case 36
(Click to view all parts)
Syncope
Preview:
Case – History
Brief History
The patient was a middle-aged Caucasian woman with past medical history of hiatal hernia, gastric ulcer (on Protonix for approximately 5 years and Mylanta) and deep venous thrombosis.
She did not visit the doctor often.
She had recent weight gain and knee pain; decreased activity and shortness of breath on exertion; and required elevation on pillows to sleep (for reflux, but possibly also for shortness of breath).
The patient also had multiple episodes of unwitnessed syncope recently where she said she woke up after passing out in the bathroom.
She was found dead after a family member could not enter her apartment and called police for a wellness check.
She was found on a couch lying on her right side.
Discussion Questions
1. What are some possible causes of death based on the history?
Back to history
Case 37
(Click to view all parts)
Alcohol use disorder and pacemaker replacement
Preview:
Case – History
Brief Past Medical History
The patient was an elderly Caucasian man with alcohol use disorder and hypertension, status post coronary artery bypass graft surgery who had a pacemaker put in approximately two years prior.
Case – History
Recent Events
Approximately 6 months prior, the patient developed a metallic taste in the mouth, prompting him to have his water supply evaluated.
Approximately 4 months prior, the patient went into renal failure, had a dialysis shunt put in and began dialysis.
Approximately 3 months prior, he fell off a chair, was admitted and found to have bulging discs.
The family remained concerned about the metallic taste, prompting evaluation of the pacemaker during the admission.
The hospital found it was “corroded.”
They removed the pacemaker and debrided the site.
At that time, a temporary external (replacement) pacemaker was placed.
The temporary pacemaker was left in place for three weeks.
The patient was hospitalized to exchange the temporary pacemaker with a permanent (internal) pacemaker.
He remained in the hospital for two weeks and then was discharged to rehab.
In rehab, he immediately decompensated, was re-admitted to the hospital and died.
He was thought to have had a heart attack in the two weeks prior to death.
The history is provided by the family.
Discussion Questions
1. Summarize the history.
2. Why were two pacemakers put in?
3. What do you think of the story that the metallic taste was due to a “corroded pacemaker”?
4. Why do you think the patient had a metallic taste?
5. What evidence in the history supports your answer?
6. What is the difference between a history provided by the family and a history provided in a medical record?
7. How strongly do you feel the family believed the pacemaker had corroded? What’s your evidence?
8. Do you think each of the patient’s procedures (removal and replacement of pacemaker) was necessary? Why or why not?
9. What do you think is the likelihood there was a medical error in this case?
10. Do you there any part of the history might have been inaccurate?
11. What are early symptoms of kidney failure?
12. Do you see any ethical considerations in this case so far?
13. Some families will pressure clinicians to take certain steps. Some clinicians can pressure themselves to comply with what they think a family wants. What kinds of threats or pressures can clinicians experience from families? Alternatively, what kinds of internal pressures can clinicians experience to “please” a family or comply with what they think the family wants? If these internal or external pressures result in an unnecessary procedure, where is the breakdown in training? How can clinicians strengthen themselves in these situations? How might these issues apply in this case?
14. How might the second surgery have been avoided while also addressing the family’s concerns about the metallic taste?
Back to history
Case 38
(Click to view all parts)
Lung mass
Preview:
Case – History
Brief History of Present Illness
The patient was a middle-aged Caucasian man with a history of Crohn’s disease, obesity, sleep apnea, hypertension and medication-controlled atrial fibrillation who had an incidental right lower lobe lung mass identified on abdominal CT.
Multiple biopsies were negative for malignancy, with the latest biopsy aborted due to technical difficulties.
A presumptive diagnosis of cancer was made based on radiography.
Case – History
Hospital Course
The patient underwent partial right lower lobectomy using the VATS procedure with right chest tube placement.
In the immediate postoperative period, the patient developed atrial fibrillation with a rapid ventricular rate and was treated with amiodarone.
Multiple x-rays showed bibasilar atelectasis; and the development of left upper lobe density.
Pathology of the lung mass showed a necrotizing fungal granuloma.
The patient was treated with IV antifungal medication and converted to oral antifungal medication.
The patient was discharged home after approximately one week.
Case – History
Home events
At home, he had persistent diarrhea and diaphoresis for several days.
He underwent cardiopulmonary arrest.
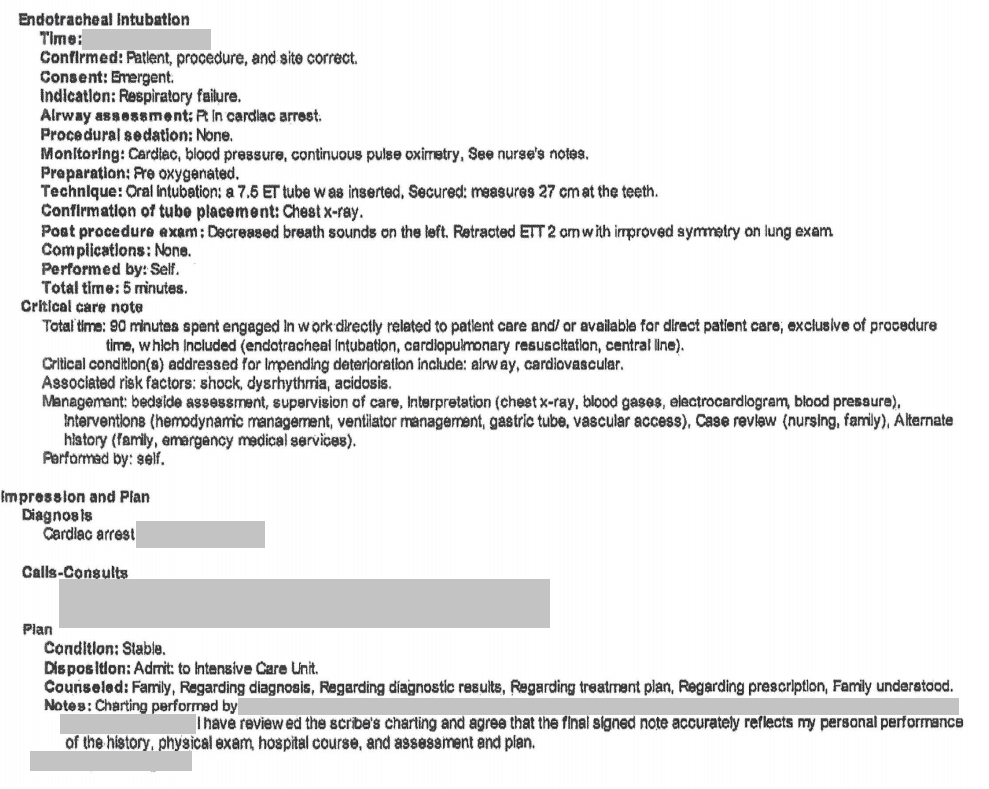
Case – History
Paramedic care
Paramedics were called who performed CPR, gave epinephrine and intubated the patient.
He was brought into the emergency room.
Case – History
Emergency room events – physician note
Page 1
![]()
Page 2
![]()
Page 3
![]()
Page 4
![]()
Page 5
![]()
Case – History
Emergency room events – nursing notes
Note 1
![]()
Note 2
![]()
Case – History
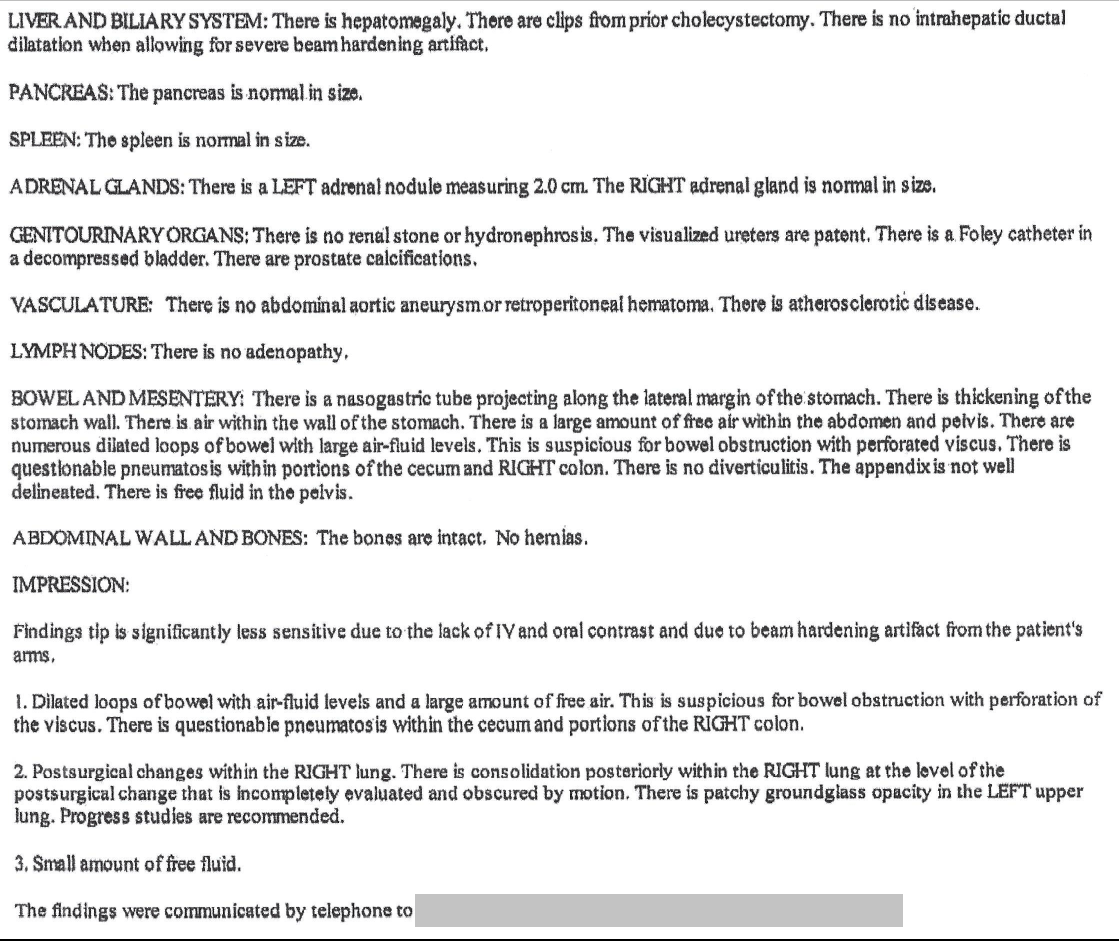
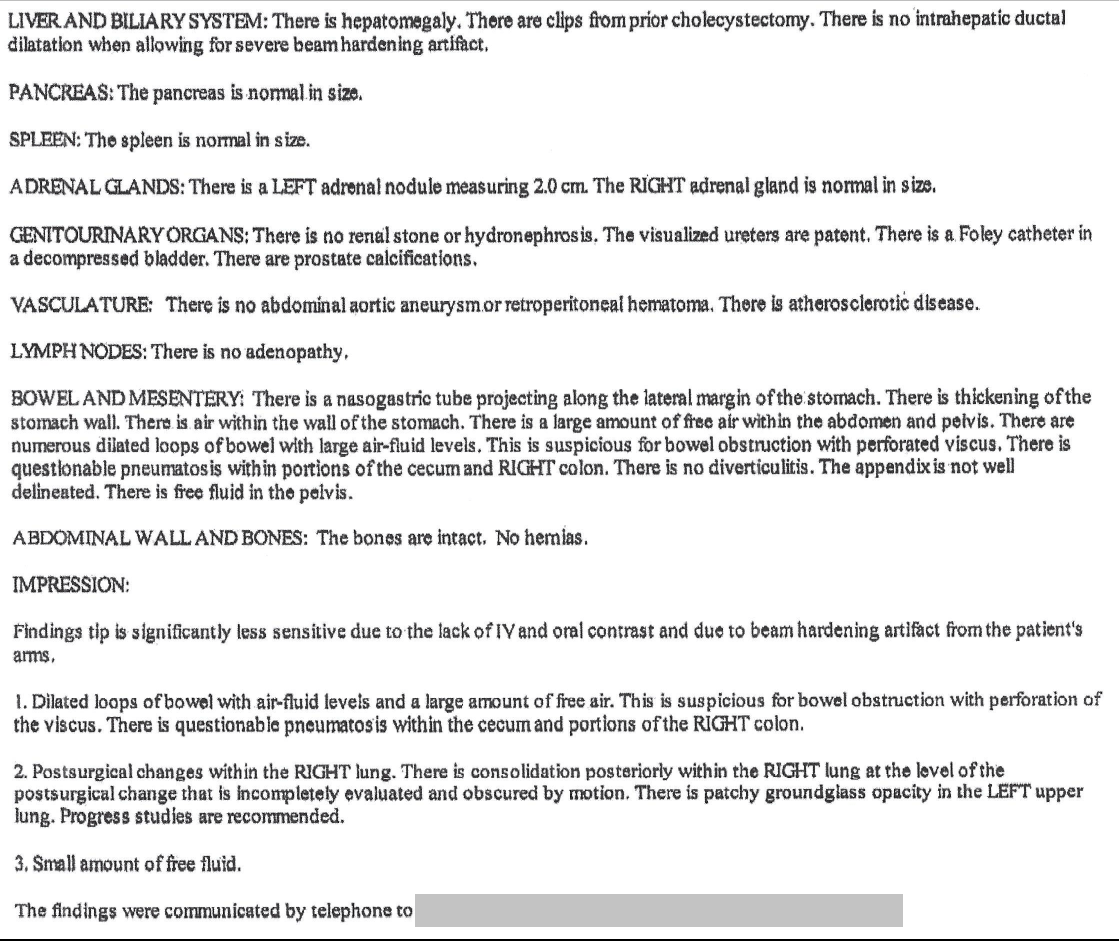
CT Abdomen and Pelvis without contrast (report from emergency room records)
Page 1
![]()
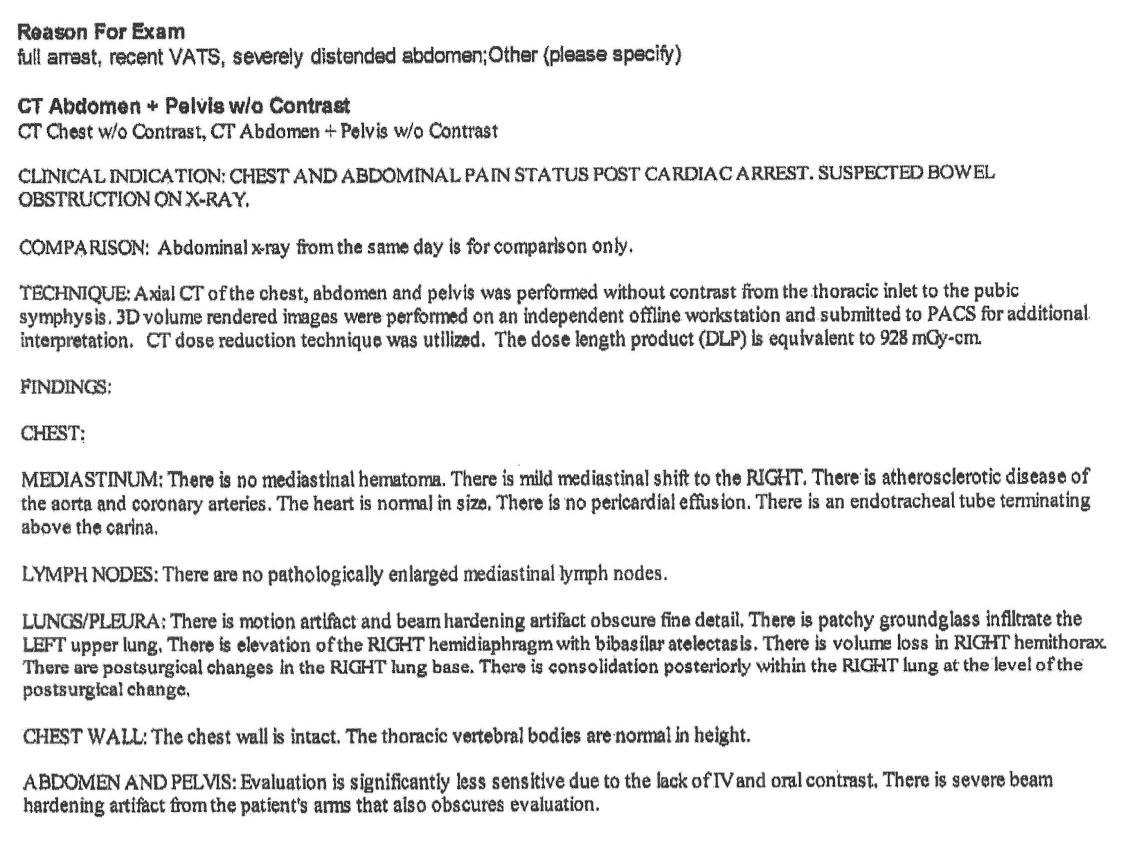
Page 2
![]()
Case – History
Emergency room events, continued
The patient despite resuscitative efforts.
Discussion Questions
1. Summarize the history.
2. Based on the history, what do you anticipate are risk factors in the patient’s death?
3. Based on the history, what organs do you suspect might have pathology related to the cause of death?
4. Based on the history, what organs do you suspect might remain normal despite the patient’s illness.
Back to history
Case 39
(Click to view all parts)
Sudden collapse; alcohol use disorder (recovering)
Preview:
Case – History
Brief Presenting History
The patient was a middle-aged Latino man, “recovering alcoholic” (per the family) with cirrhosis and esophageal varices (status post gastrointestinal bleed in somewhat recent past) and diabetes (diet-controlled in past with recent addition of oral medication).
During the prior three days, he participated in home improvement activities requiring exertion (carpentry, lifting).
On the day of death, he began to complain of dizziness, sat down, was offered something to drink and then passed out.
A family member who was a health professional was present and noted a slow pulse.
Paramedics were called and the patient was brought to the emergency room.
There was no history of slurred speech prior to his initial collapse.
Case – History
Emergency room course
The patient was intubated, and chest compressions were continued.
An echocardiogram did not show any abnormality.
The family was present and noted increased abdominal girth during resuscitation.
Resuscitation was discontinued after one hour and the patient died.
Discussion Questions
1. Summarize the history.
2. What causes of death was the patient at risk for based on the history?
3. How do you interpret information from a health professional who is also a family member? When do you consider this reliable? When might you have questions about the reliability? Do you believe the patient was bradycardic at home?
4. What is the differential diagnosis of dizziness with bradycardia? With tachycardia?
5. What is the differential diagnosis of increasing abdominal girth when it occurs chronically over time? Acutely (prior to presentation)? During resuscitation? Specifically, during CPR? Specifically, during intubation?
6. Is there a scenario where the size of the abdomen could have started to increase before resuscitation, but was only noticed at the time of resuscitation? What scenario might that be? Revisit this question after viewing the videos. Decide if it’s still relevant. State what data in the history and videos support your answer.
7. What is the purpose of mentioning slurred speech?
Back to history
Case 40
(Click to view all parts)
History of smoking
Preview:
Case – History
Past Medical and Surgical History
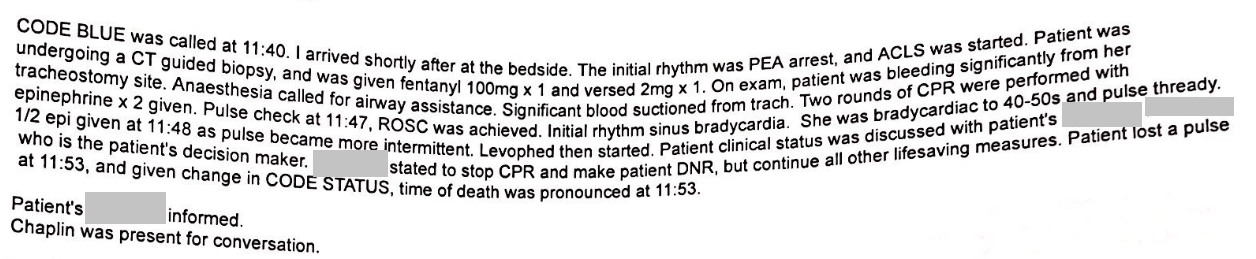
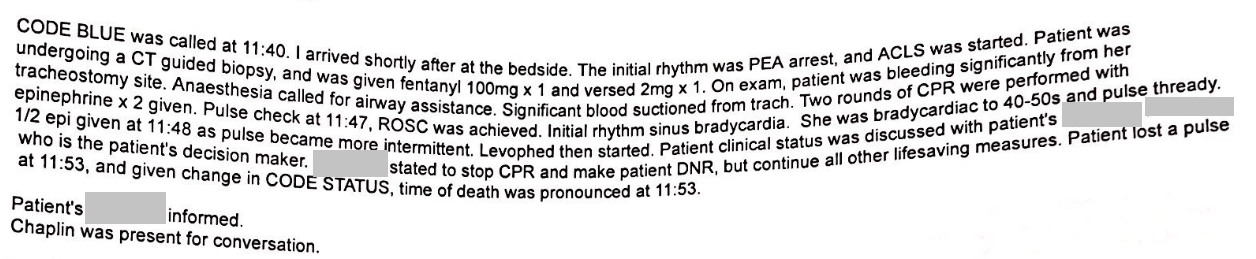
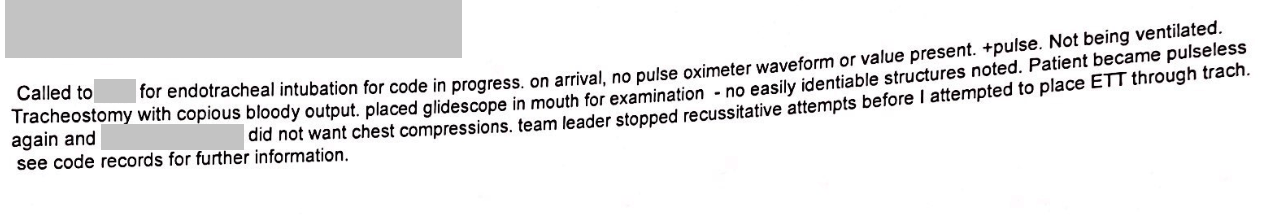
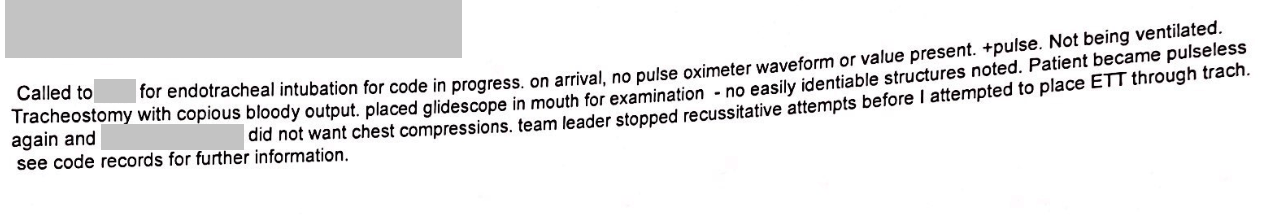
The patient was an elderly Caucasian woman, past smoker, who had lung cancer approximately 15 years prior status post left upper lobectomy and quit smoking at that time; and laryngeal cancer approximately 10 years prior status post laryngectomy complicated by tracheoesophageal fistula requiring partial esophagectomy and intestinal auto-transplant and also requiring numerous muscle grafts for local reconstruction of the tracheostomy site.
Case – History
Brief Presenting History
She was recently diagnosed with a lateral right middle lobe mass and underwent fine needle aspiration and core biopsies.
Case – History
Procedure Note
Page 1
![]()
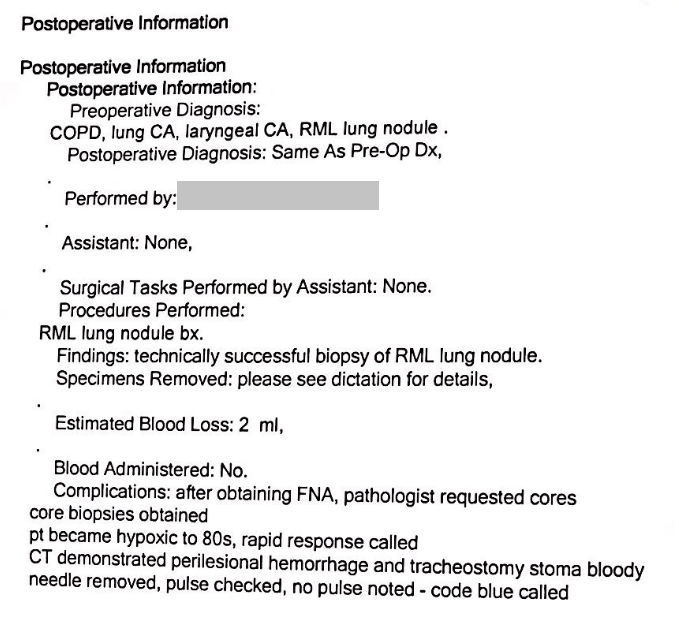
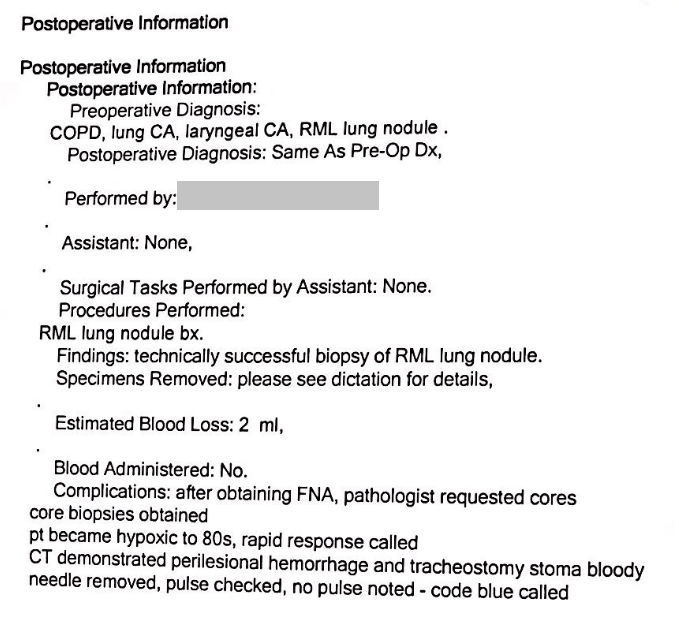
Page 2
![]()
Case – History
Code Blue note (distortion from FAX)
![]()
Case – History
Anesthesia Note (distortion from FAX)
![]()
Case – History
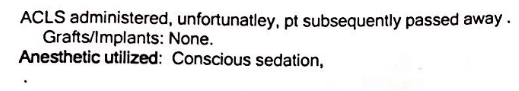
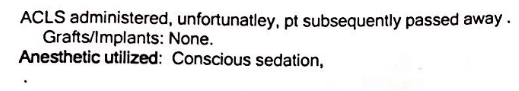
Death
The patient died during resuscitation in decision with the family.
The history is obtained from the family.
Discussion Questions
1. Summarize the history.
2. How many different cancers did the patient have? Where were they?
3. Why did the patient have so many cancers?
4. How many different procedures did the patient have? What were they? Which were diagnostic? Which were for cancer resection? Which were to restore body function? Which were for post-operative complications?
5. Do you think the initial lung cancer and the later lung mass are related? If so, how?
6. What is the likelihood of a new metastasis years after an initial lung cancer is resected? What is the likelihood of a second, new lung cancer after a first?
7. What are common ways patients with lung cancer die? Which are gradual? Which are catastrophic events? What is the anatomic basis of each?
8. How would you incorporate end-of-life discussions into your care of cancer patients? At what point in the care would you have this discussion?
9. What unique discussions might you have with a patient with a central vs. peripheral tumor?
10. What are the risks of tumor biopsy?
11. How does the risk of cancer change after cessation of smoking?
12. What are the risks of a tracheostomy procedure?
13. How is an intestinal autotransplant performed?
Back to history
Case 41
(Click to view all parts)
Recent weight gain
Preview:
Case – History
Brief Past Medical History
The patient was a middle-aged Caucasian woman with diabetes on a variable insulin regimen and weighing approximately 180-190 lbs. near the time of death (although heavier in past); borderline hypertension; status post hysterectomy (2003 for ovarian cancer), cholecystectomy, appendectomy, and umbilical hernia repair with removal of umbilicus; status post “nonmoving” deep venous thrombosis in the legs six years prior.
There is a history of deep venous thrombosis in the father.
Case – History
Recent Events
The patient had rapid weight gain from water buildup in the past approximately 2 months.
She was admitted to the hospital approximately one month prior for stress (“adrenaline,” per family) and a productive cough.
Work-up included a cardiac evaluation which was “not perfect” but showed “nothing significant.”
She was managed medically with resulting weight loss and transferred to rehab.
Case – History
Home course
At time of discharge from rehab, the family notes she was 10 lbs. heavier than her weight upon admission to rehab; and also left rehab with a “cut on the leg.”
They also reported that they were told the patient needed new, additional medications.
They reported these new medications were not ordered nor provided to them, despite their efforts to follow up.
The patient spent the week with receiving her usual (prior) medications, but not any of the new medications.
Within a week of discharge from rehab, the patient had a witnessed cardiopulmonary collapse at home.
Paramedics were called.
The patient received unspecified advanced life support measures but died.
This history is provided by the family.
Discussion Questions
1. What is your assessment of the history?
2. What is the differential diagnosis of fluid weight gain?
3. The history is provided by the family. How can you tell which parts might be more reliable and which parts might be less reliable?
4. What is the differential diagnosis of a cause of death here?
5. What conditions on your list would be dependent on receipt of medications?
6. Whose responsibility is it to ensure the patient leaves rehab with prescriptions?
7. How do you interpret the family’s self-efficacy given that an entire week passed without them getting the new, required medications? Would they be “right” to blame the physician for being unable to get ahold of the new medications?
8. What steps can a family take with an “unresponsive” provider? What other interpretations are there than that the provider was “unresponsive”? What practical, procedural, accidental or inadvertent reasons might cause a provider to seem “unresponsive”?
9. If, on further exploration, the provider stated that she provided the necessary prescriptions to the family at the time of discharge, how would this change your interpretation of the history? Would you think the family was lying? What other interpretations might there be?
10. What role might guilt or anger play in a family’s decision to request an autopsy (when they are responsible for the care of a loved one, but the loved one dies)?
Back to history
Case 42
(Click to view all parts)
Death during rehab
Preview:
Case – History
Brief History
The patient was an elderly Caucasian woman with history of mild hypertension, prior lower extremity deep venous thrombosis (status post inferior vena cava filter placement and on blood thinners), status post hysterectomy, gastric cancer (treated surgically) and status post splenectomy.
She was recently admitted to the hospital with a bleeding duodenal ulcer of undetermined etiology.
She was managed medically, stabilized, and transferred to a rehabilitation center.
Rehabilitation including physical therapy, which the family notes consisted of walking to the bathroom and back.
Case – History
One day before death
On the day before death, during physical therapy, she was noted to be symptomatic (unspecified) with an oxygen saturation of 80%.
She was given supplemental oxygen (2 liters) and evaluated with unspecified blood work.
A chest x-ray was ordered for the following day.
Case – History
Day of Death
On the day of death, the patient complained of abdominal pain.
At that time, her oxygen saturation was 85% while on 2 liters oxygen.
Oxygen was increased to 3 liters and 911 was called.
However, the patient collapsed, could not be revived and died.
There is no history of alcohol or cigarette use.
The history is provided by the family.
Discussion Questions
1. What is the differential diagnosis for this patient’s perimortem symptoms and cause of death?
2. What would you have done differently, if anything, as the patient’s clinician. Why?
Back to history
Case 42 – Educator Box 2
Clinical correlation. Discuss, in general, the possible significance of cardiorespiratory distress during physical therapy. How would you distinguish cardiac (ischemic) symptoms during patient activity vs. pulmonary embolization during patient activity? Review the mechanism by which deep venous thrombosis turns into pulmonary embolism (detachment of clot from site of origin and embolization to lungs). If the clot has formed in a limb (DVT), is embolization more likely during patient activity (e.g., limb motion)?
↓
↑Case 42 – Educator Box 3
Clinical judgment. Review the clinical attention this patient received the day before and the day of death (increasing oxygen, chest x-ray ordered for the next day, etc.). Decide if it was appropriate. What level of concern should there be for pulmonary embolism during rehab? What would you have done differently, if anything? Why?
↓
↑Case 42 – Educator Box 4
Clinical judgment. Revisit your discussion considering that the patient had an inferior vena cava filter. In general, what level of concern should there be for a pulmonary embolism when the patient has an inferior vena cava filter? How does the risk of pulmonary embolism in a patient with deep venous thrombosis change with the presence of an inferior vena cava filter? What is the incidence of pulmonary embolism in the setting of inferior vena cava filter? Considering the presence of the filter, revisit whether you would have done anything different in this case? Why?
↓
↑Case 42 – Educator Box 5
Clinical correlation and pathophysiology. The patient had both acute and subacute pulmonary embolism. The subacute pulmonary embolism is indicated by its adhesion (sticking) to the vessel wall (Part 3). This happens if the clot arrives at the lung before death and the body has time to begin the healing process inside the pulmonary artery. This fits for the clinical history of hypoxemia the day before death. The patient must have had pulmonary embolism around that time or sometime before. The patient’s death the following day with massive amounts of acute (non-adherent) clot in the right lung (Part 2) evidences acute pulmonary embolism on top of the subacute process.
Discuss whether there was a clinical window for intervention between the two events. And what might have been done.
↓
↑Case 42 – Educator Box 6
Clinical judgment. The patient also had a near-total occlusion of the proximal left anterior descending coronary artery (Part 5). Factor this into the discussion of cause of death. Was the coronary blockage the cause of death? (Unlikely in the setting of massive pulmonary embolism.) Was it a contributing factor in the death? (Also unlikely in the setting of massive pulmonary embolism. But a cardiac vulnerability from coronary occlusion may have been a factor in the patient’s symptomatic hypoxia the day prior to death (when the subacute pulmonary embolism likely presented clinically). Note: The history is obtained from the family and the exact nature of the patient’s symptoms the day prior is not known, although they knew the degree of hypoxia.)
↓
↑Case 42 – Educator Box 7
The case also illustrates bifid xiphoid process (Part 1, anatomic variation).
Case 43
(Click to view all parts)
Mental status change followed by hypotension
Preview:
Case – History
Brief History – Events two days prior to death
The patient was an elderly Caucasian man, nursing home patient who had an unwitnessed fall two days prior to death.
He was noted by the family to have mental status changes (somnolence and inability to bring dining utensils to his mouth while eating).
The family discussed this with nursing staff.
Nursing staff attributed the somnolence to “sundowning” although the patient previously was known always to be alert.
Case – History
Events – day of death
The patient fell again on the day of death.
This was followed by cardiopulmonary collapse.
Paramedics were called and the patient was brought to the emergency room.
Radiography showed an intracranial, subarachnoid bleed. Midline shift was noted. Extracranial blood was not noted in the study.
The working diagnosis by the hospital was ruptured cerebral aneurysm.
Operative drainage was deferred due to the patient’s age and clinical status.
The patient decompensated further that day and died.
Discussion Questions
This case is for independent assessment. There are no discussion questions.
Back to history
Case 43 – Educator Box 9
Pathology. The case is a good study of cerebral edema and its consequences. The brain is diffusely edematous, but more so on the right (Part 2) causing midline shift (right to left). Part 5 shows classic brainstem Duret hemorrhages. Have students learn what Duret hemorrhages are and their radiographic appearance. Absent (due to brain softening) is an assessment of various herniations.
↓
↑Case 43 – Educator Box 10
Forensics. The case shows a coup-contrecoup brain injury. The impact site is evidenced by the right temporal contusion (Part 2). The coup brain injury is the right cerebral subdural and subarachnoid injury (Part 4). The contrecoup injury is the left (mainly temporal lobe) subarachnoid hemorrhage (Part 4).
↓
↑Case 43 – Educator Box 11
For discussion. Pathophysiology. Part 2 at 1:10 shows a considerable amount of cerebral spinal fluid exiting the brain after transecting the pituitary stalk. (It is difficult to see in the video, but look for clear fluid flowing in the center of the video panel.) Where is it coming from? (Third ventricle.) Have students decide how to interpret this finding in light of the patient’s head trauma. Would you expect expanded or compressed ventricles in the case? Why or why not? In general, when might you expect changes in ventricular size acutely? Chronically? Might this be related to a prior condition? Why or why not?
Case 44
(Click to view all parts)
Longstanding urinary incontinence and frequency
Preview:
Case – History
Brief Medical History
The patient was an elderly Caucasian man, living independently, with diabetes and symptoms of urinary incontinence alternating with urinary frequency for approximately one year.
He was found to have an elevated PSA level 9 months prior to death.
Follow-up PSA level (6 months prior to death) showed the PSA had decreased somewhat.
The clinical plan at that time was to consider biopsy should the PSA level rise again.
Case – History
Two days prior to death
During a routine clinic visit 2-days prior to death, the patient was found to have elevated blood pressure and elevated creatinine.
He was taken off metformin and prescribed an antihypertensive medication.
Case – History
One day prior to death
The next day (one day prior to death), the patient noted a severe headache and was unable to speak with his grandchildren by phone.
The family is unsure whether he could not speak due to his headache or due to some other impairment.
Case – History
Day of Death
On the day of death in the morning, he apparently passed out.
He recalls waking from this event and finding that he had urinated on himself; but does not recall losing consciousness.
Later that day, he passed out again and, upon awakening, found blood in his underwear.
At this point, he called his family and was advised to call for an ambulance (911).
Paramedics arrived and brought him to the emergency room where he was admitted.
He was found to be in renal failure with leg swelling, anemia, elevated creatinine, and an elevated BNP.
His blood pressure was noted to be normal (no longer elevated), and the patient was considered stable and not in any “crisis.”
He was sent off for an unspecified ultrasound.
The patient died later that day.
The patient’s mother lived till age 93.
The patient’s father died at approximately age 70 with a long history of unspecified heart disease including multiple “heart attacks.”
The history is obtained from the family.
Discussion Questions
This case is for independent assessment. There are no discussion questions.
Back to history
Case 45
(Click to view all parts)
Death during sleep
Preview:
Case – History
Brief Past Medical History
The patient was an elderly Caucasian man with a history of lymphoma versus pre-lymphoma (monitored with blood testing).
No treatment was offered or indicated, per the family.
In addition, the patient had prostatic hypertrophy treated with medication; hypertension treated with medication; and mildly elevated cholesterol which was diet-controlled.
The diet was reported as “healthy, with many vegetables, fish and occasional meats.”
The patient also had sleep apnea and used a CPAP device (at his discretion) and a sleep apnea monitor.
Case – History
Recent Events
The CPAP device had been broken and unusable for approximately the past two weeks.
The patient had received a second shingles vaccine approximately one week prior to death.
The patient was in his usual state of health, shoveling snow approximately two days prior.
He was found dead in his bed by the family in the afternoon.
Case – History
Additional information/data provided by the family
No pill bottles were identified nearby.
The patient’s sleep-wake audio recording was provided for Review by the family.
The audio indicated that the patient was asleep during the time of his death.
There was a period of approximately 10 seconds of marked snoring followed by a brief pause and then two agonal, deep, snoring breaths prior to cessation of breathing and death.
The patient did not awaken during this time period.
Per monitoring, the death occurred overnight several hours after the patient went to sleep.
This history is obtained from the family.
Discussion Questions
1. Summarize the history.
2. What is your differential diagnosis for the cause of death?
3. What recent events may have precipitated or contributed to the death? Why?
4. Based on the history, predict what findings you might expect inside the body.
Back to history
Case 46
(Click to view all parts)
Pacemaker and chronic back pain
Preview:
Case – History
Brief Past Medical History
The patient was a middle-aged Caucasian man with a history of borderline hypertension and borderline high cholesterol who had a pacemaker placed within the past couple to several years.
The indication for pacemaker placement, per the family, was that the patient was tired or dizzy upon standing or exertion; and was found to be unable to raise his heart rate.
The pacemaker seemed to help some, but the patient still had, at least at times, some symptoms.
He also had chronic back pain.
Case – History
Recent events
Approximately 1 week prior to death, he had the sudden onset of a “new back” pain in a “different” location.
He received medical attention at least two times and with consideration for musculoskeletal back pain.
The patient himself thought the pain was some type of musculoskeletal pain.
During the two days prior to death, the patient “decompensated.”
Case – History
Day of Death
On the day of death, the family received a call from the pacemaker service asking them to bring the patient into the emergency room because they noticed a problem with the device.
The patient presented to the emergency room and underwent cardiopulmonary arrest.
Resuscitative measures were undertaken, but the patient died.
The history is obtained from the family.
Discussion Questions
1. What is your assessment of the history?
2. What treatment issues does the case illustrate?
3. Do you think the patient had musculoskeletal pain?
4. In a patient with chronic pain, how will you distinguish an exacerbation of the condition from other, more life-threatening clinical developments?
5. What is your opinion of “drug seeking behavior” in patients with chronic pain, for example, patients with sickle cell disease?
6. What is your threshold for narcotic prescription in patients with chronic pain?
7. What is the family’s and patient’s role in the health care system? Do you think the patient was “at fault” here in any manner?
Back to history
Case 47
(Click to view all parts)
Middle-aged woman status post remote hysterectomy
Preview:
Case – History
Brief History of Present Illness
The patient was a middle-aged African American woman with history of morbid obesity, hypertension, and status post remote hysterectomy for fibroid uterus, who presented with abdominal pain and constipation. She was seen as an outpatient and prescribed laxatives. The symptoms did not resolve, and, after a few days, the patient reportedly began vomiting stool.
Case – History
Hospital Course
She was admitted to the hospital and diagnosed with a complete bowel obstruction. An abdominal mass was identified radiographically.
Case – History
First Operation
The patient underwent a left hemicolectomy with ostomy placement. The mass was biopsied intraoperatively and found to be benign. The post-surgical course was complicated by necrosis of the skin at the ostomy site with dehiscence.
Case – History
Second Operation
The ostomy site was repaired during a second operation in which the necrotic skin was removed, and the ostomy site revised. The main abdominal incision was left open (instead of surgically closed) and packed.
Case – History
Remaining Hospital Course
The post-operative course was next marked by ongoing heart failure. This was managed medically, including with extensive fluid support. (The family notes “fluid coming out of the open surgical wound.”) The patient remained critically ill for the next five days and then died.
Discussion Questions
1. How do you interpret the history?
2. What is the likely reason the patient developed a bowel obstruction?
3. What is the likely etiology of the “mass” in the abdomen?
4. How common is this scenario?
Back to history
Case 48
(Click to view all parts)
Death during dialysis
Preview:
Case – History
Brief Past Medical History
The patient was a middle-aged African-American woman with a history of polycystic kidney disease requiring dialysis.
The patient had multiple surgical dialysis access sites created over time (left arm shunt, left leg shunt, right arm arteriovenous fistula).
Case – History
Recent History
Recently, she had two episodes of bleeding from the right arm arteriovenous fistula during dialysis.
For the second episode, she received transfusions.
No therapeutic or surgical treatments were made to the arteriovenous fistula.
Case – History
Day of Death
The patient had a third episode of bleeding from her right arm arteriovenous fistula during dialysis resulting in her death.
The history is obtained from the family.
Discussion Questions
1. How do you interpret the history?
2. What is polycystic kidney diseae?
3. What is the difference between a dialysis graft and an arteriovenous fistula?
4. Why might patients need multiple dialysis access sites? Is this common?
5. Given that the patient was using the right arm arteriovenous fistula during dialysis, what can you presume about the other two access sites (i.e., do you think they were functional or not)?
6. Why might a arteriovenous fistula bleed?
7. How do you interpret the patient’s care plan?
8. The amount of bleeding is not specified. How much bleeding do you think there was during the second episode? What’s your evidence?
9. Is there a scenario where the overall care plan was appropriate?
10. Thinking of the patient as your own, what might you have done differently?
Back to history
Case 49
(Click to view all parts)
Dedifferentiated liposarcoma status post resection
Preview:
Case – History
Brief presenting history
The patient was an obese, middle-aged Caucasian man who presented with one month of abdominal pain and swelling, and left testicular pain.
The patient’s presenting weight was approximately 300 lbs.
Abdominal CT scan showed a large left retroperitoneal mass measuring approximately 24 cm in maximal dimension.
Biopsy diagnosis was dedifferentiated liposarcoma.
Case – History
Initial course.
Over the next month, the patient developed decreased appetite and approximately 30 lb. weight loss.
Pre-operative CT Abdomen Pelvis With Contrast
![]()
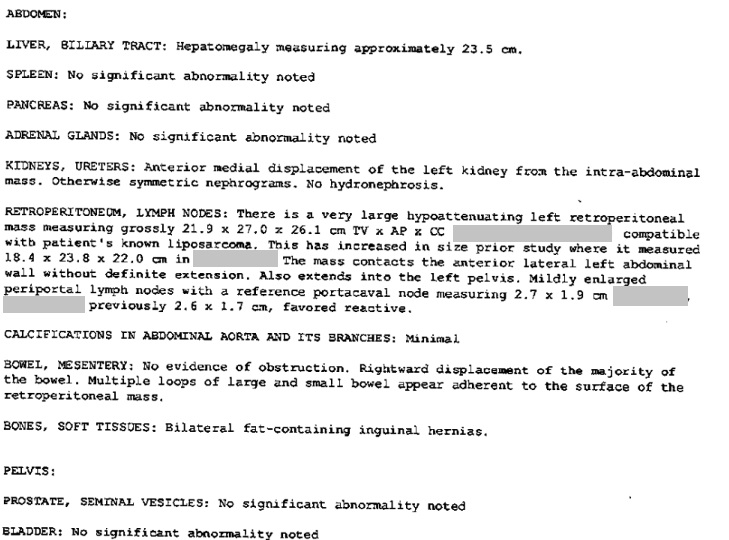
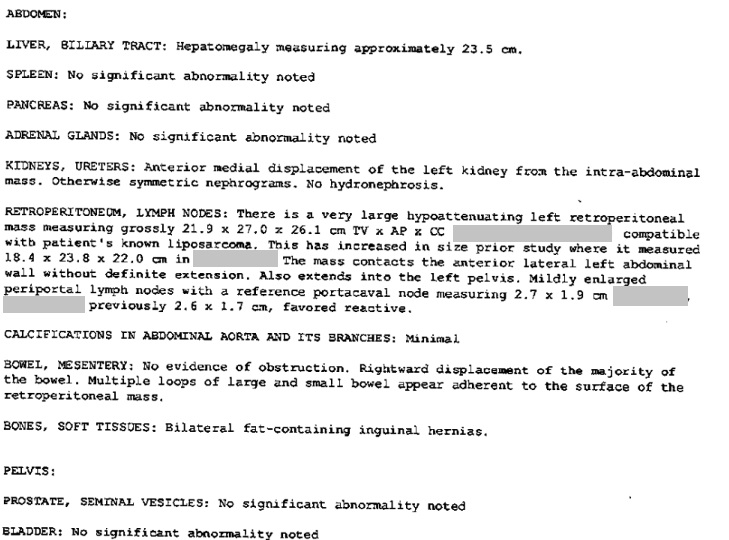
Case – History
Surgery and immediate posteperative course
The patient underwent operative resection approximately 2 months after diagnosis.
The surgery and immediate post-operative period were unremarkable.
Case – History
Post-operative course (continued)
The patient developed abdominal swelling and inability to defecate.
He was noted to have bowel dilatation, radiographically.
He was then found to have bilateral pulmonary embolism and was transferred to the ICU.
Case – History
Death
Repeat radiographic studies were concerning for recurrent tumor.
The patient was admitted to hospice, then transferred home where he died.
The time between initial diagnosis and death was approximately 6 months.
Discussion Questions
1. What is a dedifferentiated liposarcoma?
2. How do you interpret the history?
3. What postoperative complications did the patient have?
4. What could have caused each of the complications?
5. Sort through the timing of the complications. What does the timing tell you about the possible causes of each complication?
Back to history
Case 50
(Click to view all parts)
Death after coronary stenting
Preview:
Case – History
Presentation
The patient was an elderly African American man with diabetes, hypertension and unspecified cardiac disease treated with multiple medications including diuretics.
The patient did not take his diuretic medicine for two weeks during which time he developed bilateral leg swelling.
He went to a covering physician who advised the patient to return home and elevate his legs.
The leg swelling worsened and the patient was admitted to the hospital.
Case – History
Initial hospital course
The patient was treated with diuretics.
This decreased the leg swelling on the left.
The swelling remained on the right and worsened with weeping through the skin.
The patient had concurrent symptoms of bradycardia.
Case – History
Later hospital course
Three days after admission, the patient had a cardiac catheterization which showed blockage of the right coronary artery.
The blockage was “severe” and stented with two “small stents.”
Case – History
Day of death
The following day, the patient underwent cardiopulmonary arrest.
He received advanced cardiac life support measures but died.
The history is obtained from the family.
Discussion Questions
1. What symptoms of heart failure did the patient have?
2. What is the differential diagnosis of bradycardia?
3. Can coronary artery disease cause bradycardia? How?
4. Can bradycardia cause symptoms of congestive heart failure? How?
5. Does the location of the patient’s blockage explain all of the patient’s symptoms? Why or why not?
6. Would you have performed the cardiac catheterization?
7. What other testing would you have requested in this case?
8. Why do you think the patient died?
9. Do you think the patient would have died without the procedure?
Back to history
Case 51
(Click to view all parts)
Sudden death in rehab – in development
Preview:
Case in development
The purpose of this case is to show a brain dissection. Stay tuned for updates.
Discussion Questions
1. Identify standard brain internal anatomy in the video.
Back to history
Case 52
(Click to view all parts)
Sudden death after knee arthroscopy
Preview:
Brief History
The patient was an elderly Caucasian man who underwent outpatient arthroscopic surgery of the right knee three weeks prior.
The surgery was uncomplicated.
Within two days post-operatively, the patient was up, active and working.
He reported improved right knee function.
On the day of death, he complained of abdominal swelling and pain.
The following day, he was found deceased with red-brown emesis emanating from his mouth and along his right face, right neck and right chest.
The patient self-medicated with non-steroid anti-inflammatory medication of unknown amount after the surgery.
There was minimal alcohol use.
The patient was a smoker.
The history is obtained from the family.
Discussion Questions
In development.
Back to history
Case 53
(Click to view all parts)
Premature rupture of membranes
Preview:
Brief History of Presentation
The patient was an African American infant born at 25 weeks gestation after premature rupture of membranes and premature labor.
Delivery
Upon delivery, the patient was responsive, initially with good respirations and oxygenation.
However, in minutes, he developed increasing oxygen requirements and apnea.
He was orally intubated.
A chest x-ray was performed to confirm position of the tip of the endotracheal tube.
This was found to be in the right mainstem bronchus.
The tube was pulled back approximately 0.3 cm.
Hospital day 2
Follow-up chest x-ray was performed.
The x-ray showed the tip of the endotracheal tube at the carina.
The x-ray also showed the development of right upper lobe “airspace disease.”
The endotracheal tube pulled back approximately 1.5 cm.
Hospital day 3
Follow-up chest x-ray was performed.
This showed increasing “airspace disease” in the right upper lobe and new, patchy disease in the rest of the lungs.
There was concern for right upper lobe collapse.
This was managed by progressive increases in the ventilator tidal volume; and by positioning the patient left side down (right side up).
These maneuvers achieved normal oxygen levels through the following day.
Hospital day 4
The patient underwent a trial of extubation.
He quickly decompensated.
An x-ray showed “complete opacification of the right hemithorax. There is diffuse airspace disease in the left lung as well. This is significantly worse than previously a day earlier.”
The patient was re-intubated.
The re-intubation was complicated by bilateral pneumothoraces.
He received additional life-saving measure, but died.
Search options
