Case 2
Diabetes, stroke, feeding tube
Preview:
Please login, activate your subscription,
or explore access solutions.
Brief History of Present Illness
The patient was a middle-aged African American man with insulin-requiring diabetes (with multiple admissions for diabetic ketoacidosis), stroke (with immobility and difficulty swallowing, requiring gastrostomy and jejunostomy tube placement), hypertension and dementia who was noted to have a high blood glucose and lethargy as well as shortness of breath and cough for a couple days.
Home Events
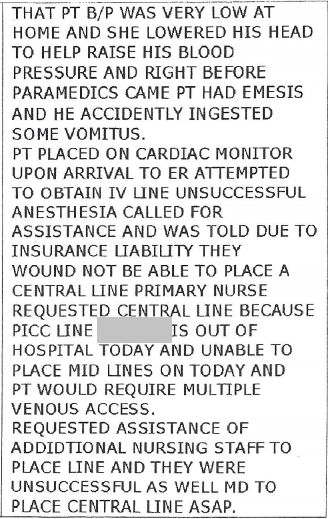
The wife took his blood pressure, which was “very low,” lowered his head to help raise his blood pressure and called paramedics.
Right before they came, the patient vomited.
The wife was concerned he accidentally “ingested” some vomitus.
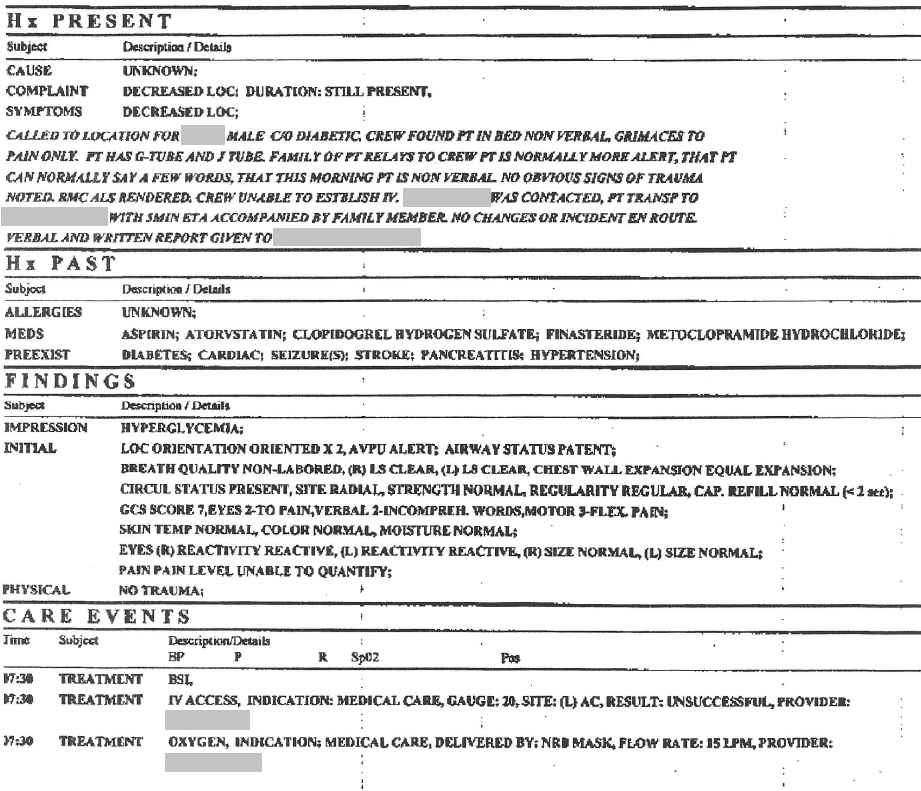
Paramedic Notes
Page 2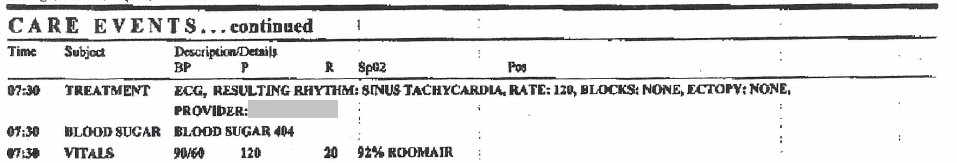
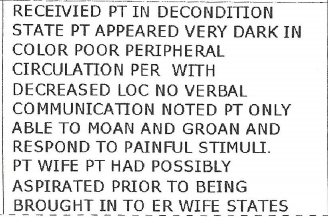
Emergency Room Note
Additional Emergency Room Note
Intubation was difficult requiring three attempts with varying size endotracheal tubes.
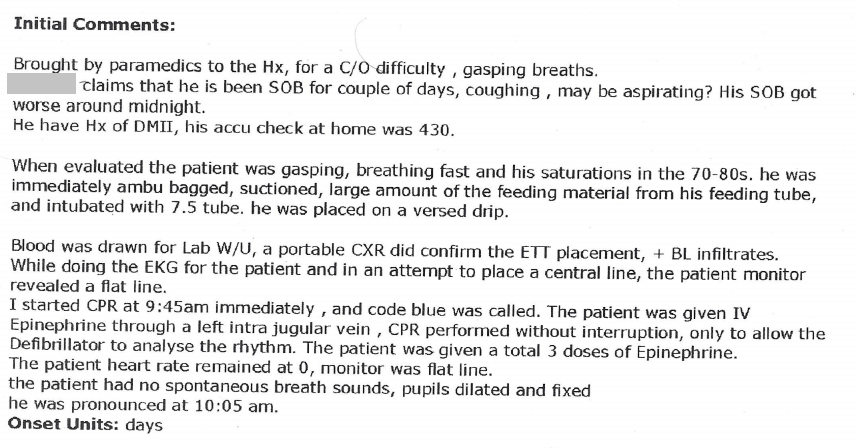
Additional Emergency Room Note
Page 2
Additional Emergency Room Note
The patient died in the emergency room.
Discussion Questions
1. Summarize the medical history.
2. What was the patient’s status upon arrival of paramedics?
3. What was the patient’s status during transport?
4. What was the patient’s status in the emergency room?
5. Looking at questions 2, 3 & 4, are there any discrepancies? If so, how do you account for them? (See medical records.)
6. What choices affected the patient’s care starting from home through to the emergency room?
7. Are there any choices that were intended to help but which may have led to worsening of his condition? If so, which?
8. What is your opinion on “assigning fault” in a death? How would you talk with someone who intended to help a patient, but ended up harming them? What if this were a family member? Does any of this apply to this case? How?
9. What ethical issues are raised in the medical record titled “View additional emergency room note”?
10. The history states there were three attempts at intubation. What factors can make intubation difficult? List ones that are related to the patient. List ones that are related to the provider.
11. Create your own definition of what it means to be a “competent” health care provider.
12. Can you imagine an adverse outcome with “competent care”? If so, describe the scenario you have in mind.
13. Come back to questions 1 – 12 after studying the videos and decide if you wish to revise any of your answers.
