Case 28
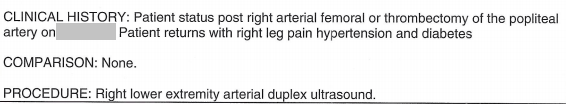
Peripheral vascular disease and recent angioplasty
Preview:
Please login, activate your subscription,
or explore access solutions.
Brief History of Present Illness
The patient was a middle-aged Latina woman with history of right lower leg pain she initially thought was an insect bite.
Initial assessment
On presenting for medical care, she was found have to peripheral vascular disease.
Initial (Pre-operative) Angiogram
Pre-operative Echocardiogram
Hospital course
She underwent an emergency thromboembolectomy of the right femoral, popliteal, anterior tibial and right tibioperoneal trunk arteries; and patch angioplasty of the right popliteal artery.
The pain was mildly improved after the procedure.
Five days postoperatively, she developed blisters and pain at the surgical site and was diagnosed with reperfusion syndrome.
After a number of days, she was discharged home still in considerable pain.
Second admission
She returned to the emergency room approximately 2 week later in severe, intolerable pain localized to the right lower leg and was admitted.
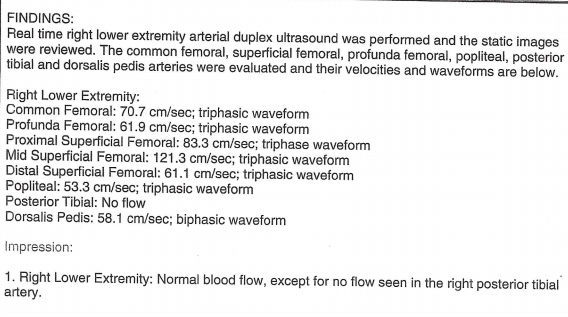
Right lower extremity venous doppler report – second admission
Part 1
Part 2
Emergency room physician note – second admission
Part 1
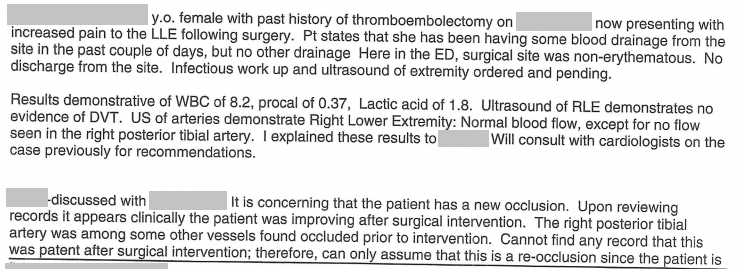
Part 2
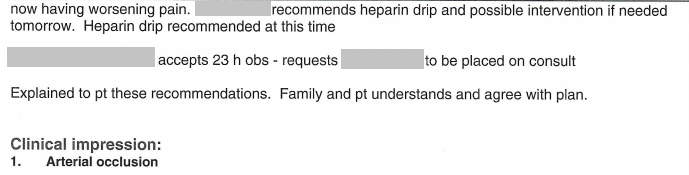
Hospital course – second admission
On admission, she was tachycardic.
The patient had a second vascular procedure of the right leg (atherectomy of right posterior tibial artery and balloon angioplasty of right anterior tibial artery).
Intraoperative angiogram – second surgery
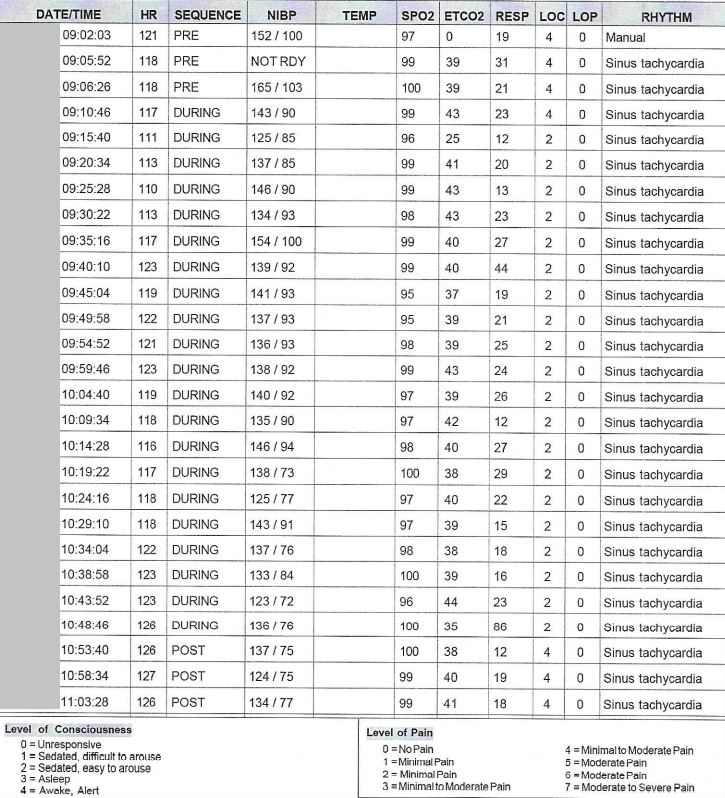
Intraoperative vital signs – second surgery
Additional hospital course – second admission
Within several days post-operatively, she developed shortness of breath and died.
Discussion Questions
1. Summarize the history.
2. Review the initial angiogram. What vascular structures can you identify? Which are patent? Which are occluded. Construct a diagram to show which arteries are patent, which are occluded, and by how much.
3. Review and assess the preoperative echocardiogram.
4. The history indicates three major decisions: the first operation, the hospital discharge, and the second operation. Evaluate each based on the clinical data. Which decisions do you agree with? What would you do differently? What additional information might be helpful?
5. If you had chosen to discharge the patient after the first operation, what would your discharge instructions have looked like?
6. What are the systemic consequences of ongoing pain? Did the patient manifest any of these?
7. Review the emergency room studies and emergency room physician note. What did the venous doppler find? What did the arterial study find? How did the arterial study compare to any prior studies according to the physician note?
8. Evaluate the emergency room physician’s logic in determining the cause of the patient’s pain. Do you agree? Come back to this question after viewing all the videos. Has your assessment changed? If so, why?
9. The emergency room physician documents the word “presume” in the medical record. When is this kind of thinking acceptable in clinical care? Can you give an example of when it is? When it is not? When is it dangerous to make presumptions or assumptions in medicine? Is it ever safe to make a presumption or assumption in medicine? Come back to this question after viewing all the videos. Have your answers changed? If so, why?
10. Even if you do not agree that it is acceptable to make a presumption, does the data support the kind of presumption the physician made? Why or why not?
11. You are the provider. Your patient’s condition worsens, yet available studies remain unchanged. How do you interpret this? How will you proceed? What resources can you draw on? (Revisit this question after studying the case videos.)
12. What are some likely reasons this patient could have died?
13. Come back to the history after viewing all the parts of the case. Reassess the clinical data in light of what you know about the patient’s anatomy and condition. Do you think there were any medical errors? If so, what were they? What data could you review to support your thinking? Do you think there was one error by one person? Or multiple errors by multiple people? Was this a diagnostically difficult case? Or were the errors more easily avoidable? What training issues present here?
14. What is your attitude towards medical errors? Does it depend on the type of error? The outcome? If you think there were errors in this case, what types of errors were there? Is one type more “correctable or preventable” than another? Which could be addressed systemically? Intradepartmentally? Individually?
